Do you want BuboFlash to help you learning these things? Or do you want to add or correct something? Click here to log in or create user.
Growth
#has-images #ir #peds
- GROWTH
- Failure to Thrive: cross 2 %-tiles, wt <3%-tile, <80% ideal body wt
- A 14yo ♂ with 1y Hx of FTT. He is pale and has diffuse abdominal pain. What are possible causes? What are 5 tests you would do to narrow your differential?
- DDx: non-organic, celiac, IBD, CF, T1DM, haematologic, malignancy, liver disease, obstructive uropathy
- Ix: CBC/Fe, celiac screen (tTGT), lytes, urea, Cr, TSH, U/A, Ca2+, Vit ADE
- 14yo at 3rd %ile weight + 10th %ile height is not eating well. What are 3 possible causes?
- See above
- A full term baby presents with an eating disorder (i.e. FTT). What is your DDx?
- ↓intake: non-organic, GERD, structural, CNS, genetic
- ↓absorption: CF, CMPA, short gut, biliary atresia, GI
- ↑loss: gastroenteritis
- ↑demand: cardiac, ↑THY, infection, respiratory
- Ineffective use: inborn error of metabolism
- Obesity
- 14yo ♂ with weight of 67 kg, height 150cm.
- Calculate BMI: 29.8 kg/m2
- 4 complications of obesity: HTN, dyslipidemia, OSA, SCFE, nonEtOH fatty liver
- 3 tests to perform for obesity: lipids, GLUC, HbA1c, ALT/AST, liver U/S
Weight
• At birth = 3.0‐3.5kg (avg)
• Normal to lose up to 10% of birth weight in first 4‐7 days
o BUT should return to birth weight no later than 10‐14 days
• Doubles birth weight by 4‐6 months; triples birth weight by 1 year
• Quadruples birth weight by 2 years
Head Circumference
• At birth = 35cm (avg)
o <32cm small head = small brain until proven otherwise
• May be inaccurate at birth due to caput succedaneum, molding
• 0‐3mths = +2cm/mth
• 3‐6mths =+1cm/mth
• 6‐12mths = +0.5cm/mth
Height
• At birth = 50cm (avg)
• Doubles height by 4 years
• Measure recumbent length until 2 years, then standing height
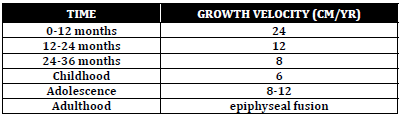
Normal Growth Velocity
Growth Charts
• Critical to use gender and age appropriate growth charts
• In 2010, the CPS, RCFPC and the Dieticians of Canada, recommended
the use of the 2006 WHO Growth Standards and Reference charts
• WHO Growth Standards based on longitudinal data from solely breast
fed for first six months, healthy children from diverse ethnic and
geographic backgrounds; use BMI after age 10.
• Growth charts are also available for premature infants and certain
syndromes
• Use corrected age up to 2 years for plotting premature infants
Failure to Thrive
Definition
• Weight < 3%ile (the further below the curve the more likely to be
pathologic in origin)
• Weight falls across major %ile lines
• Weight < 80% of ideal body weight*
* use appropriate growth charts for gender and certain genetic conditions
Factors Affecting Physical Growth
• Genetics
• Intrauterine factors
• "Internal time clock"
• Nutrition
• Endocrine hormones
• Chronic infections/diseases
• Psychosocial factors
Etiology
• Inadequate intake: insufficient provision of food, vomiting, oro‐motor
dysfunction
• Inadequate absorption: pancreatic insufficiency, celiac disease
• Increased utilization: chronic diseases, hyperthyroidism
• Ineffective utilization: chromosomal disorders
• Increased losses: chronic diarrhea, urinary losses
Differential Diagnosis
Nonorganic/
Psychosocial
Most common cause of FTT, often seen in conjunction with organic FTT
Specific Organic Diseases
• Genetic: Turner/Downs/Russell Silver Syndrome, FAS, TORCH
• Cardiac: Chronic cardiac failure
• Pulmonary: Recurrent or chronic infections, Cystic Fibrosis
• GI: GERD, vomiting, IBD, chronic liver disease, malabsorption
syndromes (Celiac Disease, CF, Schwachman Diamond syndrome)
• Renal: Chronic renal failure, obstructive uropathies
• Endocrine: Hyperthyroidism, hypopituitarism, DM‐1, DI
• CNS: Difficulty coordinating swallow, MR, CP, Diencephalic Syndrome
• Haematology: Chronic hematologic disorders, malignancies
• Inflammatory/Immune: SLE, immunodeficiencies
Risk Factors
Child Factors
• Premature, low birth weight
• Feeding, sleep or elimination problems
• Recurrent illness
• Developmental delay
Parental Factors
• Parents abused or neglected as children
• Unwanted, unplanned pregnancy
• Marital problems, single parent
• Drugs/alcohol
• Young inexperienced parents
• Unwell/stressed parent
• Poor follow‐up, uncooperative parents
• Misconceptions of eating habits and nutrition
Child and Parental Factors
• Difficulty feeding, refusal to feed
• Colic, sleep problems
• Behavioural issues
• Parent not able to recognize child’s needs and respond to child’s cues
Environmental Factors
• Low SES, unemployment
• Lack of support, social isolation
• Lack of access to consistent medical care
History
• Duration of problem, detailed dietary and feeding history, appetite,
behavior before and after feeds, BM history, vomiting
• Pregnancy, birth, birth weight, postpartum history, developmental
history, growth patterns
• Family patterns of growth including parental heights and age of
puberty
• Current illnesses, symptoms, past medical history
• Family relationships, detailed social history
• Assess child’s temperament, child‐parent interaction, feeding
behaviour, parental psychosocial issues
Physical Exam
• Ht/Wt/HC‐ plot on growth chart; compare to prior values
• HR, RR, BP
• Complete general physical examination
Investigations/Imaging
• Use your history and physical exam to guide your choice of
investigations
• Consider investigations to look for etiology and investigations to assess
for other deficiencies
• CBC, lytes, urea, creatinine, TSH, T4, U/A, celiac screen, vitamin A,D,E,
ferritin, calcium
• Consider karyotype, microarray, bone age (AP x‐ray of L hand and
wrist) if also short stature
Management
• Treat underlying cause
• Provide education about age‐appropriate foods, mealtime scheduling
and behaviour
• Caloric fortification of food
• May need referral to dietitian, social work
Overweight and Obesity
Introduction
• Growth monitoring should be performed at primary care visits for
children and youth ages 17 and younger
• BMI = mass (kg) / height (m2)
o WHO Growth Charts for Canada are recommended which have
different cutpoints for the definition of overweight and obesity
than the US‐based CDC charts
• Cut‐off points for overweight and obese depend on age and BMI (WHO)
o Birth to 2 years
‐ Risk of overweight – Weight for length > 85th
‐ Overweight – Weight for length > 97th
‐ Obese – Weight for length > 99.9th
o 2 to 5 years
‐ Risk of overweight – BMI > 85th
‐ Overweight – BMI > 97th
‐ Obese – BMI > 99.9th
o 5 to 19 years
‐ Overweight – BMI > 85th
‐ Obese – BMI > 97th
‐ Severely obese – BMI > 99.9th
• Over 60% of overweight children will have at least one CV risk factor
History
• What concerns, if any, do you have about your child’s weight? When
did weight gain start? Has gain been slow over time or sudden?
• What, if any, past attempts at weight loss have been made?
• Review of systems for comorbidities and etiologies of obesity:
o Headaches, blurred vision (hypertension, intracranial
hypertension)
o Breathing pauses when sleeping, snoring, daytime sleepiness (OSA)
o Joint pain (slipped femoral capital epiphysis, blount disease)
o Menstrual history, hirsutism, acne (hyperandrogenism, PCOS)
o Polyuria, nocturia (T2DM)
o Increased fatigue, cold intolerance, constipation, dry skin
(hypothyroidism)
o Stunted growth, striae (Cushing’s)
• Family History
o Identify obesity in first degree relatives
o Evaluate history of cardiovascular disease, type 2 DM, cancer in
first degree or second‐degree relatives
• Diet
o Identify caretakers who feed the child
o Identify foods high in calories and low in nutritional value that can
be reduced, eliminated, or replaced
o Assess eating patterns (e.g. timing, content, location of meals and
snacks)
o Estimate the type and quantity of beverage intake (sugar
sweetened beverages, juice, pop)
o Frequency of dining out
• Activity
o Identify barriers to walking or riding a bike to school
o Evaluate time spent in play
o Evaluate school recess and physical education (frequency, duration
and intensity)
o Assess after‐school and weekend activities
o Assess screen time (television, computer, movies, video games)
• Assess psychological impact of weight on child (bullying, depression,
anxiety, social isolation etc.)
Physical Exam
• Obtain and plot weight, height, BMI on WHO Growth Charts for Canada
Complete physical exam
• Findings to look for
o Hypertension
o Enlarged thyroid
o Acanthosis nigricans (insulin resistance)
o Striae
o Hepatomegaly
o Hirsutism
o Hip/knee pain or decreased ROM (Blounts, SCFE)
o Sexual maturity rating
Investigations
• Investigations can be performed for children who meet cut‐off point
for obesity
• Lipid profile, glucose, HbA1C
• Liver enzymes (specifically ALT) every 2 years
• Consider ultrasound of liver if liver enzymes are abnormal
• Fasting lipid profile every 2 years
• Fasting plasma glucose, HbA1C every 2 years, if severe obesity
(consider 2 h OGTT (1.75 mg/kg upto max 75 g)
• Sleep study if symptoms present
Management
• Structured behavior programs should not be offered to children/youth
who are at a healthy weight to prevent obesity
• The subject of talking about a patient’s weight can often be a very
sensitive topic.
o Ask for permission to discuss weight
o Assess obesity related risk and potential ‘root causes’of weight gain
o Advice on obesity risks, discuss treatment benefits and options
o Agree on a realistic SMART plan to achieve health behavior
outcomes
o Assist in addressing drivers and barriers, offer education and
resources, refer as necessary and arrange follow‐up
• Stress the importance of achieving behavioural and health‐related
improvements rather than focusing primarily on numbers on a scale.
• Behaviour modification – can produce weight loss of 5‐20% over 3‐6
months
• Lifestyle modification strategies can be broadly categorized as:
o Controlling the environment – include the entire family in healthy
changes rather than child alone
o Monitoring behavior
o Assessing motivation
o Setting realistic goals
o Rewarding successful changes in behavior
o Arrange short‐term follow‐up to review progress
• Involve a multidisciplinary team (dietitian, exercise therapist, social
worker, psychologist)
• There is no role of medications (such as orlistat) for healthy weight
management in children 2‐11 years old or for routine use in youth 12‐
17
• Surgical management can be offered in a select group of adolescents –
there is no role for routine referral for surgical management for
overweight/obesity
Healthy Active Living
Syllabus: Lipnowski et al. Healthy Active Living: Physical activity guidelines for
children and adolescents . Paediatr Child Health. 2012;17(4):209.
Introduction
• ‘Healthy living’ is described by Health Canada as making choices that
enhance physical, mental, social and spiritual health
• Health care professionals should be promoting physical activity and
reducing sedentary time in children and adolescents
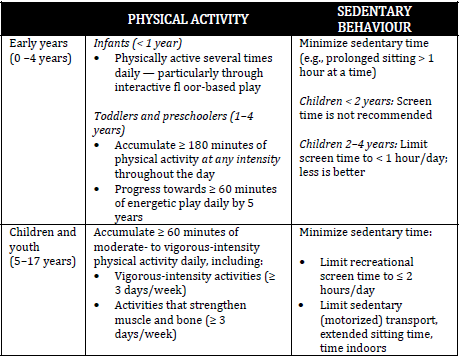
Canadian guidelines for physical activity and sedentary behavior
Short stature: differential ABCDEFG:
Alone (neglected infant)
Bone dysplasias (rickets, scoliosis, mucopolysaccharidoses)
Chromosomal (Turner's, Down's)
Delayed growth
Endocrine (low growth hormone, Cushing's, hypothyroid)
Familial
GI malabsorption (celiac, Crohn's)
If you want to change selection, open original toplevel document below and click on "Move attachment"
Summary
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Details
Discussion
Do you want to join discussion? Click here to log in or create user.