Do you want BuboFlash to help you learning these things? Or do you want to add or correct something? Click here to log in or create user.
Development
#has-images #ir #peds
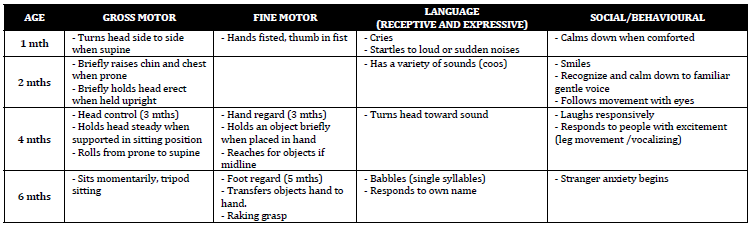
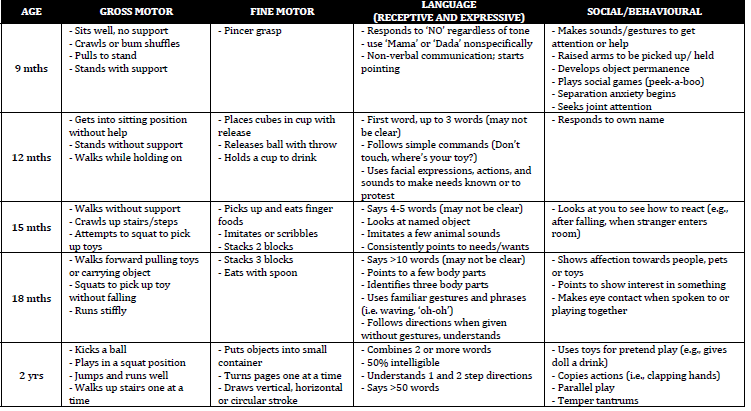
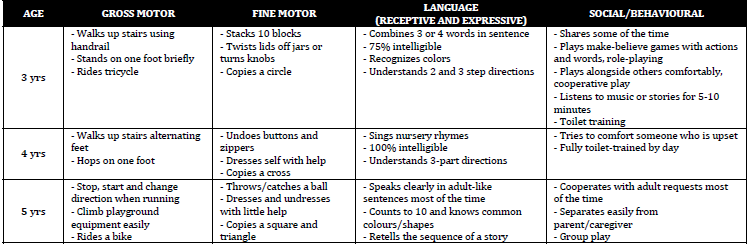
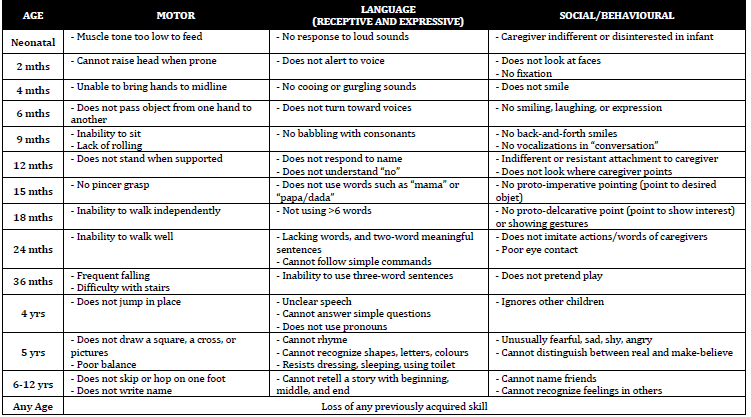
- DEVELOPMENT [See chart]
- NORMAL
- Case on child not toilet training: what is the likely reason?
- Not yet interested in learning how, i.e. few signs present (requires physiologic, communication, psychologic)
- 5yo has been developing normally, but his father has been concerned he's been showing poor speech. What's the first Ix to do?
- MCQ: audiology testing, NOT genetic testing
- Developmental milestones for 6mo.
- Normal: tripod sits, pivots in prone position, reaches/grasps objects, brings toy to mouth, babbles, squeals when excited, grunts in anger, stranger anxiety starts
- Lists developmental progress for a 12mo, what type of delay does this child have - language, fine motor, gross motor, or global delay?
- Normal: gets into sitting position without help, stands without support, walks while holding on, neat pincer grasp, places cubes in cup with release, releases ball with throw, says 2-3 words, understand simple requests and questions, uses facial expressions/actions/sounds to make needs known, responds to own name, separation anxiety begins
- 3 yo development milestone (circle 8): I guess the biggest lesson I took away with me from this exam is from the key features section and this question in particular: listen to what your predecessors have to say about the exam in the past exams you see in this email account! When I saw, in one of the previous peds exam, that one is required to pick things out of a list of 20 development milestones, none of which appears in Toronto Notes, I did not take the warning seriously, and I'm forced to pay for my irreverence. I randomly circled 8 things and would be lucky if I can walk away with half the marks. So the lesson is that not only should you remember the short list of developmental milestones from Toronto Notes or the Peds handbook you got from year 2 for the short answers part, but you should also remember a longer, more exhaustive list of milestones from some other source for the key features version of the development milestonesànot true in 2015
- Normal: walks upstairs using handrail, stands on one foot, rides tricycles, stacks 10 blocks, twists lid off jars, copies a circle, combines 5 or more words in a sentence, understands 2-3 step commands, recognizes colours, shares willingly some of the time, make-believe games, plays with others, listens to music or stories for 5-10 minutes, jumping on one foot, washes and dries own hands, dresses self independently except shoe laces, knows own sex, tells detailed stories, knows primary colours, speaks with plurals
- Pick developmental milestones from a list (I think for a 3yo and another one for a 4yo?)
- See above
- Developmental Milestones achieved by 15 mo? 18mo? What about 6-10 yrs? 16 wks?
Developmental Milestones
There are four main areas of developement – gross motor, fine motor, language and social. All areas should be explored when exploring a
developmental history. The milestones cited are, on average, those at the 50th percentile for age.
Developmental Problems
Differential Diagnosis
• Motor
o Problems with CNS (e.g., Cerebral palsy)
o Problems with PNS (e.g., Muscular dystrophy)
o Metabolic conditions (e.g., Hypothyroidism)
o Genetic syndromes (e.g., Down Syndrome)
• Language
o Structural/functional abnormalities of oromotor anatomy
o Hearing impairment
o Pure language disorders
o Pervasive developmental disorders (e.g., Autism Spectrum
Disorder)
• Cognitive
o Global developmental delay due to:
- Genetic conditions (e.g., Fragile X)
- Deprived environment
- Prenatal/perinatal events leading to brain anoxia/ischemia
(rare)
- Prenatal exposures (e.g., Fetal Alcohol Spectrum Disorders)
• Emotional/Social
o Pervasive developmental disorders (e.g., Autism Spectrum
Disorder)
o Deprived environment
Management
• Motor
o Educate parents about poor correlation between motor delays and
intelligence
o Refer to Physiotherapy and Occupational therapy
o Educate parents on developmental targets and techniques for
helping achieve specific milestones
- e.g. adequate ‘Tummy Time’ to facilitate development of head
control, rolling over, etc.
• Language
o Audiology assessment
o Referral to local early intervention services
o Speech and language (SLP) evaluation
o Enroll child in nursery school
o Educate parents regarding language facilitation techniques
- make noises or sing and repeat sounds the child says
- ask questions/make comments that lead to a response
- label objects and emphasize action words
- read to the child
- use simple, slow language
• Cognitive
o Thorough history:
- Pregnancy (obstetrical history, exposures, complications)
- Birth (gestational age, complications, delivery, resuscitation)
- Family History (parents, siblings, consanguinity)
- Social History (identify deprived environments)
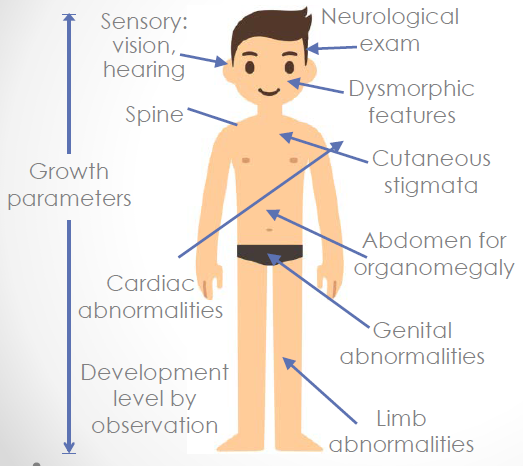
o Physical exam including head growth, dysmorphic features,
neurologic exam
o Hearing/vision assessment
o Other tests as indicated: karyotype, blood lead levels, metabolic
screen, TSH, CT/MRI
o Find appropriate schooling/community living
o Help family find support groups, funding, respite
• Emotional/Social
o Early intervention with early intervention therapists
o Provide opportunities for increased contact with other children e.g.,
play groups, structured daycare
o Refer to specific therapeutic groups
o If applicable, remove child from deprived environment with help of
children’s aid society
Developmental Surveillance
Rourke Baby Record
Available in the Syllabus and through the CPS website at:
www.cps.ca/english/statements/CP/Rourke/RBROntario.pdf
• Evidenced based health supervision guide for health care providers
caring for children 0‐5 years old
• Specific version for physicians in Ontario to include information for the
enhanced 18 month visit and a guide to the Ontario Early Childhood
Development and Resource System
• Includes sections for:
o Growth and nutrition
o Nutrition
o Development milestones – to aid developmental surveillance, not a
screen. Set after time of normal milestone acquisition.
o Anticipatory guidance
o Physical examination
Enhanced 18Month
WellBaby
Visit
Syllabus: Canadian Task Force on Preventative Health Care. Recommendations on
screening for developmental delay. CMAJ. 2016; 188(8):579.
• Important time to review child’s developmental domains and
achievement of milestones
• Visit should incorporate use of Rourke Baby Record, screening for
parental morbidities (mental health, physical illness), promotion of
literacy activities (reading, singing), and information about resources
• Standard developmental screening tools (eg: Nipissing) no longer
recommended for children whose parents or clinicians have no
concerns regarding delay
• Screening still appropriate in children presenting with
signs/symptoms, or parental concerns of delay.
Greig Health Record
Available in the Syllabus and through the CPS website at:
www.cps.ca/english/statements/CP/PreventiveCare.htm
• Evidenced based health promotion guide for health care providers
caring for children and adolescents aged 6 – 17 years
• Guide for periodic health visits, recommendations and discussion
points grow along with patient.
• Similar to Rourke Baby Record.
• Includes sections for:
o Weight, height, BMI
o Psychosocial history and development
o Nutrition
o Education
o Behaviour and family issues
o Injury prevention and safety
o Physical examination
o Guidelines and resources (eg: vaccinations)
Attention Deficit/Hyperactivity Disorder
Syllabus: Floet et al. Attention Deficit/Hyperactivity Disorder. Pediatrics in Review.
2010;31(2):56.
American Academy of Pediatrics. ADHD: Clinical Practice Guideline for the
Diagnosis, Evaluation and Treatment of Attention‐Deficit/Hyperactivty Disorder in
Children and Adolescents. Pediatrics. 2011;128(5):1007.
Introduction
• ADHD is a neurobehavioral disorder defined by symptoms of
inattention, hyperactivity, and impulsivity.
• There is a two‐ to three‐fold higher prevalence in boys than girls with
girls being more likely to be diagnosed with the inattentive‐type ADHD
• Can profoundly effect academic performance, social interactions and
well being
DSM5
Diagnostic Criteria for Attention Deficit/Hyperactivity Disorder
A. A persistent pattern of inattention and/or hyperactivity‐impulsivity
that interferes with functioning or development, as characterized by
(1) and/or (2):
1. Inattention: Six (or more) of the following symptoms have persisted
for at least 6 months to a degree that is inconsistent with
developmental level and that negatively impacts directly on social
and academic/occupational activities:
a. Often fails to give close attention to details or makes careless
mistakes in schoolwork, at work, or during other activities (e.g.,
overlooks or misses details, work is inaccurate).
b. Often has difficulty sustaining attention in tasks or play
activities (e.g., has difficulty remaining focused during lectures,
conversations, or lengthy reading).
c. Often does not seem to listen when spoken to directly (e.g., mind
seems elsewhere, even in the absence of any obvious
distraction).
d. Often does not follow through on instructions and fails to finish
schoolwork, chores, or duties in the workplace (e.g., starts tasks
but quickly loses focus and is easily sidetracked).
e. Often has difficulty organizing tasks and activities (e.g., difficulty
managing sequential tasks; difficulty keeping materials and
belongings in order; messy, disorganized work; has poor time
management; fails to meet deadlines).
f. Often avoids, dislikes, or is reluctant to engage in tasks that
require sustained mental effort (e.g., schoolwork or homework;
for older adolescents, preparing reports, completing forms,
reviewing lengthy papers).
g. Often loses things necessary for tasks or activities (e.g., school
materials, pencils, books, tools, wallets, keys, paperwork,
eyeglasses, mobile telephones).
h. Is often easily distracted by extraneous stimuli (for older
adolescents, may include unrelated thoughts).
i. Is often forgetful in daily activities (e.g., doing chores, running
errands; for older adolescents, returning calls, paying bills,
keeping appointments).
j. Hyperactivity and impulsivity: Six (or more) of the following
symptoms have persisted for at least 6 months to a degree that
is inconsistent with developmental level and that negatively
impacts directly on social and academic/occupational activities:
a. Often fidgets with or taps hands or feet or squirms in seat.
b. Often leaves seat in situations when remaining seated is
expected (e.g., leaves his or her place in the classroom, in the
office or other workplace, or in other situations that require
remaining in place).
c. Often runs about or climbs in situations where it is
inappropriate. (Note: In adolescents, may be limited to feeling
restless.)
d. Often unable to play or engage in leisure activities quietly.
e. Is often "on the go," acting as if "driven by a motor" (e.g., is
unable to be or uncomfortable being still for extended time, as
in restaurants, meetings; may be experienced by others as being
restless or difficult to keep up with).
f. Often talks excessively.
g. Often blurts out an answer before a question has been
completed (e.g., completes people's sentences; cannot wait for
turn in conversation).
h. Often has difficulty waiting his or her turn (e.g., while waiting in
line).
i. Often interrupts or intrudes on others (e.g., butts into
conversations, games, or activities; may start using other
people's things without asking or receiving permission; for
adolescents, may intrude into or take over what others are
doing).
B. Several inattentive or hyperactive‐impulsive symptoms were present
prior to age 12 years.
C. Several inattentive or hyperactive‐impulsive symptoms are present in
two or more settings (e.g., at home, school, or work; with friends or
relatives; in other activities).
D. There is clear evidence that the symptoms interfere with, or reduce the
quality of, social, academic, or occupational functioning.
E. The symptoms do not occur exclusively during the course of
schizophrenia or another psychotic disorder and are not better
explained by another mental disorder (e.g., mood disorder, anxiety
disorder, dissociative disorder, personality disorder, substance
intoxication or withdrawal).
Types
• Combined presentation: If both Criterion A1 (inattention) and
Criterion A2 (hyperactivity‐impulsivity) are met for the past 6 months.
• Predominantly inattentive presentation: If Criterion A1
(inattention) is met but Criterion A2 (hyperactivity‐impulsivity) is not
met for the past 6 months.
• Predominantly hyperactive/impulsive presentation: If Criterion A2
(hyperactivity‐impulsivity) is met and Criterion A1 (inattention) is not
met for the past 6 months.
Risk Factors
• Genetic factors: heritability is approximately 75%
• Nongenetic factors: perinatal stress and low birth weight, traumatic
brain injury, maternal smoking during pregnancy, severe early
deprivation
Physical Exam
A physical examination is important in ruling out underlying medical or
developmental problems such as the following:
• emotional or behavioral (eg. anxiety, depression, oppositional defiant
and conduct disorders)
• developmental (eg. learning and language disorders or other
neurodevelopmental disorders)
• physical conditions (eg. tics, sleep apnea)
Examination should include observation of the child and the parent and
their relationship.
Investigations
• Laboratory and imaging studies are not routinely recommended.
However, consideration of hearing and vision tests, thyroid function
studies, blood lead levels, genetic karyotyping and brain imaging
studies if indicated by past medical history or physical examination
• In most cases, laboratory investigations will not be necessary
• Consider a psycho‐educational evaluation including both cognitive and
academic testing to assess for learning problems
Management
Syllabus: Belanger et al. Cardiac risk assessment before the use of stimulant
medications in children and youth. Paediatrics and Child Health. 2009;14(9):579.
Feldman et al. Extended‐release medications for children and adolescents with
attention‐deficit hyperactivity disorder. Paediatrics and Child Health.
2009;14(9):593.
Bernard‐Bonnin A‐C et al. The use of alternative therapies in treating children with
attention deficit hyperactivity disorder. Paediatrics and Child Health.
2002;7(10):710zXXZas Paediatrics and Child Health. 2009;14(9):593.F.
• Approach to treatment is multidisciplinary
• Psychoeducation and support for patient and family
• In cases of ADHD without co‐morbidity, behavioural therapies have not
been shown to be helpful for the core symptoms of ADHD
• School aged children (6‐18 yrs):
o First line is stimulant medication(s)
o Second line is non‐stimulant medications
o Third line is behavior management: positive reinforcement, time
out, response cost, token economy
• Pre‐school aged children (4‐5 yrs):
o First line is behavior management: positive reinforcement, time out,
response cost, and token economy
o Second line is stimulant medication(s)
• Dietary interventions such as the elimination of sugar have NOT
proven to have an observable effect. Other dietary interventions (i.e.,
elimination of food additives or addition of dietary supplements)
require evidence‐based research
• Follow‐up and long‐term management are required as ADHD does not
resolve with age
Medications
• Stimulants (methylphenidate, dextroamphetamine) are considered
first line because they are highly efficacious in reducing symptoms
• Extended release stimulant medications are associated with decreased
use of street drugs among adolescents with ADHD, decrease in rate of
injuries, STI’s and unwanted pregnancies
• Immediate‐release medications such as Ritalin should be avoided as
they are much easier to divert, crushed Ritalin may be snorted or made
into an injectible form, mixed with narcotics and taken as a ‘speed‐ball’
• Medications should be used 365 days per year in adolescents
• Careful titration of medication to optimize effects, minimize side effects
and enhance compliance is essential.
Autism Spectrum Disorder
Syllabus: Johnson C et al. Identification and Evaluation of Chidlren with Autism
Spectrum Disorders. Pediatrics. 2007;120(5):1183.
Harrington et al. The Clinician’s Guide to Autism. Pediatrics in Review.
2014;35(2):62.
Simms et al. Autism, Language Disorder, and Social (Pragmatic) Communication
Disorder: DSM‐V and Diferential Diagnosis. Pediatrics in Review. 2015;36(8):355.
Introduction
• The essential features of autism spectrum disorder are persistent
impairment in reciprocal social communication and social interaction,
and restricted, repetitive patterns of behavior, interests, or activities.
• These symptoms are present from early childhood and limit or impair
everyday functioning
• Social skills deficits can be noticed in infancy with aversion to cuddling
and lack of acknowledgement of the caregiver
• Also can involve language delays/deficits, motor signs (e.g.,
stereotypies, toe walking), sensory deficits (e.g., intolerance to sound)
• Cognitive abilities vary; typically difficulties with reasoning/planning,
greater abilities in rote memory
DSM5
Criteria for Autism Spectrum Disorder
A. Persistent deficits in social communication and social interaction
across multiple contexts, as manifested by the following, currently or
by history (examples are illustrative, not exhaustive; see text):
1. Deficits in social‐emotional reciprocity, ranging, for example, from
abnormal social approach and failure of normal back‐and‐forth
conversation; to reduced sharing of interests, emotions, or affect; to
failure to initiate or respond to social interactions.
2. Deficits in nonverbal communicative behaviors used for social
interaction, ranging, for example, from poorly integrated verbal and
nonverbal communication; to abnormalities in eye contact and
body language or deficits in understanding and use of gestures; to a
total lack of facial expressions and nonverbal communication.
3. Deficits in developing, maintaining, and understanding
relationships, ranging, for example, from difficulties adjusting
behavior to suit various social contexts; to difficulties in sharing
imaginative play or in making friends; to absence of interest in
peers.
B. Restricted, repetitive patterns of behavior, interests, or activities, as
manifested by at least two of the following, currently or by history
(examples are illustrative, not exhaustive; see text):
1. Stereotyped or repetitive motor movements, use of objects, or
speech (e.g., simple motor stereotypies, lining up toys or flipping
objects, echolalia, idiosyncratic phrases).
2. Insistence on sameness, inflexible adherence to routines, or
ritualized patterns of verbal or nonverbal behavior (e.g., extreme
distress at small changes, difficulties with transitions, rigid thinking
patterns, greeting rituals, need to take same route or eat same food
every day).
3. Highly restricted, fixated interests that are abnormal in intensity or
focus (e.g., strong attachment to or preoccupation with unusual
objects, excessively circumscribed or perseverative interests).
4. Hyper‐ or hyporeactivity to sensory input or unusual interest in
sensory aspects of the environment (e.g., apparent indifference to
pain/temperature, adverse response to specific sounds or textures,
excessive smelling or touching of objects, visual fascination with
lights or movement).
C. Symptoms must be present in the early developmental period (but may
not become fully manifest until social demands exceed limited
capacities, or may be masked by learned strategies in later life).
D. Symptoms cause clinically significant impairment in social,
occupational, or other important areas of current functioning.
E. These disturbances are not better explained by intellectual disability
(intellectual developmental disorder) or global developmental delay.
Intellectual disability and autism spectrum disorder frequently cooccur;
to make comorbid diagnoses of autism spectrum disorder and
intellectual disability, social communication should be below that
expected for general developmental level.
Risk Factors
• Male (4x risk)
• Having another child with autism
• Advanced parental age
• Genetic/cytogenetic/syndromic conditions
o Down Syndrome, Tuberous sclerosis, untreated PKU, Fragile X,
Angelman, Cornelia de Lange syndrome
• Early bilateral mesial temporal lobe lesions due to herpes simplex or
anoxic/ischemic damage
• Very low birth weight, especially with retinopathy of prematurity
• No association between MMR vaccination and autism
o Studies that showed causation were fraudulent
Screening
• Developmental surveillance is encouraged at all well baby/child visits
• Developmental screening at 18 month visit
• Targeted (secondary) screening is recommended in high risk children
(risk factors, parental concerns, teacher observations, missed
milestones etc) and requires use of specific screening tools (e.g. CHAT)
• Determination that a child is at high risk of ASD should result in
immediate referral to an experienced diagnostician or an
interdisciplinary assessment team
INADEQUATE LANGUAGE FEATURES SUGGESTING AUTISM
At any age
• Regression of language or communicative gestures
• Lack of reliable orienting to speech, turning to name
• Concern about language comprehension
• Persistent mutism unpredictably interrupted by rare isolated clear words or
sentences
In toddlers
• No pointing by 1 year; dragging by the hand
• No words by 12‐14 months
• Less than a dozen words by 18 months
• No 2‐word phrases by 2 years or sentences by 3 years
• Very delayed or absent head shaking or nodding to signify no/yes
In preschoolers and older children
• Failure to answer questions or responding beside the point
• Inability to use language conversationally, “talking to talk” rather than to
communicate (request, show, etc)
• Frequent, persistent verbatim repetition (echolalia)
• Persistent pronoun inversion (you/me confusion), referring to self by name
• Verbatim repetition of overlearned expressions (delayed echolalia, formulaic
speech) rather than self‐generated expressions
• Inability to recount an event or tell a coherent story
• Perseveration on a favorite topic
• Overuse of pedantic words or expressions
• High‐pitched, sing‐song, or uninflected robotic speech
Investigations
• Formal audiological assessment
o Consider blood tests: genetic (karyotype, Fragile X, 22q deletion,
microarray), metabolic, lead levels and neurologic tests: MRI, EEG
Diagnosis
• In accordance with DSM‐V Criteria
• Interdisciplinary approach is ideal
• Assessment of cognitive and developmental levels is required
• Can be diagnosed as early as 18 months by experienced professionals
• Should be made on the basis of a thorough developmental history and
structured behavioural observation and clinical judgment.
• The use of at least one standardized, norm‐referenced parent report
measure and at least one standardized, norm‐referenced behavioral
observation measure is recommended.
Management
• Early, multi‐disciplinary intervention is beneficial
• Structured learning
• Speech and language assessment and therapy
• Occupational therapy ‐ sensory integration
• Behaviour management support
• Medications for self‐injurious and aggressive behaviours
o SSRIs, psychotropic drugs (e.g., Risperidone), anticonvulsants
• Social skills training
• Vocational counseling
Note: Elimination diets and vitamins have no proven efficacy
Learning Disorders
Syllabus: Rimrodt et al. Learning Disabilities and School Failure. Pediatrics in
Review. 2011;32(8):315.
Byrd R. School Failure: Assessment, Intervention, and Prevention in Primary Care
Pediatrics. Pediatrics in Review. 2005;26(7):233.
• Represent a disability based on a descrepency between a person’s
intellectual ability and actual academic performance
• Further specificed into the particular area of academic function
affected:
o Mathematics disorder
o Reading disorder
o Disorder of reading expression
• Any child who has school problems and is suspected of having a
learning disability should be referred for a comprehensive
psychoeducational evaluation
• Accomodations can be made at school through the Identification,
Placement, and Review Committee (IPRC). The IPRC will:
o decide whether or not a student should be identified as exceptional
o identify the areas of a student’s exceptionality
o decide an appropriate placement for a student
o review identification and placement at least once per school year
• An IEP (Individual Education Plan) is developed (in consultation with
parents and the student) for each student who has been identified as
exceptional by the IPRC process. An IEP is a written plan that describes
the strengths and needs of the student, services established to meet
that student’s needs, and how these should be delivered
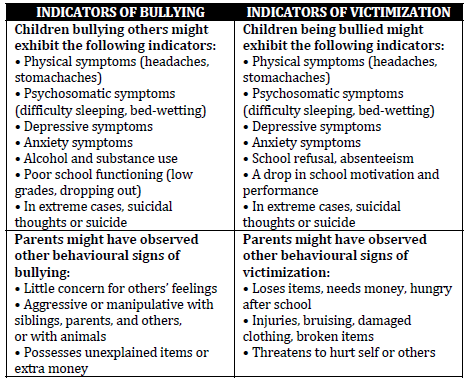
Bullying
Syllabus: Lamb et al. Approach to Bullying and Victimization. Canadian Family
Physician. 2009;55(4):356.
Introduction
• Defined as the use of power or aggression to cause distress or control
of another
• Can be direct (face‐to‐face) or indirect (gossip, exclusion)
• Negative actions can include:
o Physical actions (punching, kicking, biting)
o Verbal actions (threats, name calling, insults)
o Social exclusion (spreading rumours, gossiping, excluding)
• Actions are repeated and the intensity or duration establishes
dominance
History
• When a physician identifies a possible bullying situation, the following
questions can help determine what type of help may be appropriate
o Who do you bully/who bullys you?
o What do you do to others/what do others do to you? (e.g. gossiping,
insults, hitting, etc.)
o When and how often do you bully/are you bullied?
o Where do you bully/where are you bullied?
o Why do you bully others/why do you think you are bullied?
o How do you think the kids feel when you bully them or how do you
feel when you are bullied?
Management
• Comprehensive strategies that encompass the school, family and
community are most likely to be effective
o establish a social school environment that promotes safety
o provide access to health and mental health services
o integrate school, family and community prevention efforts
o provide training to enable school staff to promote safety and
prevent violence effectively
Toilet Training
Syllabus: Clifford et al. Toilet Learning: Anticipatory Guidance with a child‐oriented
approach. Paediatrics and Child Health. 2000;5(6):333.
Feldman. Managing primary nocturnal enuresis. Paediatr Child Health. 2005;
10(10):611.
Bayne et al. Nocturnal enuresis: An approach to assessment and treatment. Peditrics
in review. Pediatrics in Review. 2014; 35(8):327.
Austin et al. Dysfunctional Voiding. Pediatrics in Review. 2000;21(10):336.
Har et al. Encoperesis. Pediatrics in Review. 2010;31(9):368.
Signs of a child’s toilet learning readiness
• Can understand and follow simple instruction
• Diaper is consistently dry for 2 to 3 hours at a time or after naps
• Bowel movements are somewhat regular and predictable
• Seems uncomfortable with soiled diapers and wants to be changed
• Recognizes and tells or shows need to urinate or stool
• Can walk to bathroom and pull pants up and down
• Is stable on potty (good trunk support)
• Interested and motivated to learn how to use the potty
• Shows interest in 'big kid' underwear
- Child does not need to show all of the signs, but at least a few should be
present to indicate the child is ready for toilet training
- Average age for a child to be toilet trained is between 2 to 3 years old
- Advise parents to expect accidents during initial training
Sleep Requirements
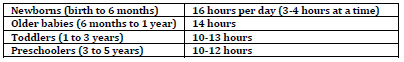
Newborns
• Should sleep on back in crib with flat surface, no pillows or soft items
• In parents’ room for first 6 months
Older babies
• Maintain regular daytime and bedtime schedule
• Start consistent bedtime routine
• Avoid putting baby to bed with a bottle
Sleep Problems
Night terrors
• Parasomnia that occurs in first third of night
• High to extreme autonomic agitation
• High arousal threshold, agitated if awakened
• No daytime sleepiness or recall of event
Nightmares
• Occur in last third of night during REM sleep
• Mild to high autonomic arousal/agitation
• Low arousal threshold, agitated after event
• Can have daytime sleepiness and frequent, vivid recall of event
• Very common
BEARS Screening Tool for Pediatric Sleep Disorders
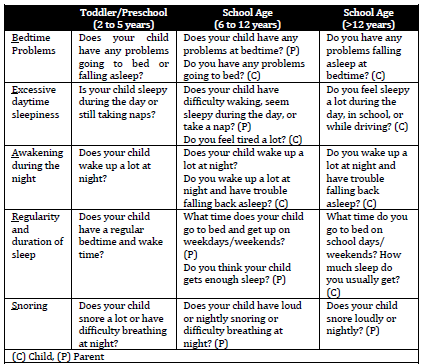
Sleep associations
• Infant or toddler child has learned to fall asleep only under certain
conditions or has specific sleep associations that require parental
intervention, such as being rocked or fed, which are usually readily
available at bedtime
• During the night, when the infant or toddler awakens, they are not able
to get back to sleep ("self‐soothe") unless those same conditions are
available
90
o The infant then "signals" the caregiver by crying or coming into the
parents' bedroom if the child is no longer in a crib until the
necessary associations are provided
o Ferber method advocates that at bedtime child is put in bed while
they are drowsy, but still awake, to help them learn how to fall
asleep on their own (self‐soothe)
Colic
Syllabus: Cohen et al. Colic. Pediatrics in Review. 2012;33(7):332.
• Infantile colic is defined as
o paroxysms of irritability, fussiness or crying that start and stop
without obvious cause;
o episodes lasting 3 h or more per day and occurring at least three
days per week for at least three weeks; and
o no failure to thrive
• Peaks at 6 weeks of age and typically ends by 3‐4 months
• Crying is most frequent in the late afternoon or evening
• Holding or rocking and offering a pacifier might help
• There is no evidence that medicines really help with colic
• There is no or insufficient evidence to support dietary changes
including probiotics, lactose free diet, soy formulas
• If there is a concern about cow’s milk protein allergy, a time limited
(two week) trial of hypoallergenic formula or elimination of cow’s milk
from the maternal diet can be undertaken
Gotta Find Strong Coffee Soon
•Gross Motor
•Fine Motor
•Speech/ Language
•Cognitive
•Social Emotional, Behaviour
•(Adaptive Skills)
Approach to Developmental History
-History of presenting illness
-Perinatal history (TORCH inf's)
-Past medical history
-Hearing, vision, sleep, feeding
-Developmental history (-start asking from several age groups lower than current age; observe child)
-Family history (developmental delay, learning disabilities
metabolic/genetic conditions
consanguinity)
-Social history (typical day, language spoken at home, other children at home, daycare/preschool, child maltx/CAS, income, etc)
physical exam
•Weight, height and head circumference at 50th percentile (want to know if macro/microcephaly, any dysmoprhic ft's
make sure to undress & look at skin)
•Low, posteriorly rotated ears but no other dysmorphic features or unusual birth marks
•Normal general and neurologic examinations
GLOBAL DEVELOPMENTAL DELAY
Significant delay (at least two standard deviations below the mean with standardized tests) in at least two developmental domains from the following:
Gross or fine motor
Speech/ language
Cognition
Social/ personal
Activities of Daily Living
-Child must be less than 5 years old
Causes of GDD/ID
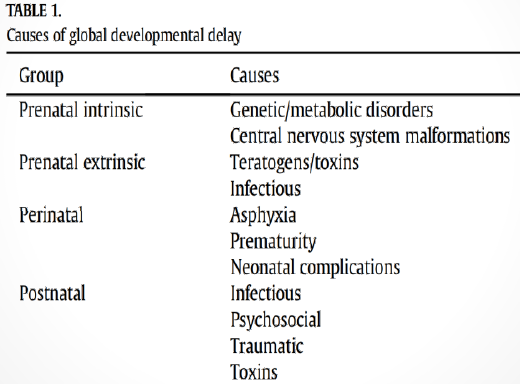 .
.Pediatric milestones in development
1 year:
-single words
2 years:
-2 word sentences
-understands 2 step commands
3 years:
-3 word combos
-repeats 3 digits
-rides tricycle
4 years:
-draws square
-counts 4objects
Stairs mnemonic. Two at two. One at four.
Two feet on each step at two years. One foot per step at four years.
Birth to 1 Year: Remember that the goal of the first year is to be able to walk (walk at 12 months). At six months you are halfway there (remember “sit at six”). Just with these two milestones you can pretty much fill in everything else. Remember that everything is from head to toe. So 2 months (the first time we really check milestones) you check for head lifting (neck control). You roll at 4 months (at level of shoulders and chest). Then, again, at six you sit. You crawl at 9 months and pull to stand (crawl, pull to stand at 9 months) which makes sense as being between sitting and walking.
In Review:
2 months: lift head 45 degrees
4 months: roll over (front to back first, then back to front, easier if you can push off with hands)
6 months: sit (halfway to goal, halfway through year, “sit at six”)
9 months: crawl, stand (halfway between sitting and goal)
12 months: walk (the goal)
15 months – 5 years: Memorize these milestones in a story as they are harder to associate with particular months like the first year. Using this progression story may help you.
15 months: walks well
18 months: throws objects
24 months/2 years: up and down stairs (one foot at a time); run
3 years: Tricycle (3 wheels, 3 years), jump in place
4 years: up and down stairs alternating feet (2 feet x up/down = 4), balance on 1 foot for 4 seconds (legs look like a 4 when on 1 foot), hop
5 years: skip (5 looks like an “S”kips)
Story: a child on the 1st floor of her house sits up, crawls, cruises, then 1) WALKS to stairs, 1.5) THROWS object up stairs, 2) CLIMBS up the stairs and RUNS to his trike, 3) RIDES a trike upstairs, JUMPS off, 4) RUNS down the stairs, HOPS off the stairs and 5) SKIPS away
3. Once you’ve memorized the months of well child checks and corresponding gross motor milestones, begin to memorize the archetype babies for each age group. These little stories incorporate all the other milestones into a single image which is much easier than trying to memorize many unrelated facts. There are some ways to conceptually link milestones across categories, but they are not frequent enough to be useful for fast recall and the salient milestones and timing which is what happens on tests and during morning report.
Here are all the babies with milestones listed:
2 months: lift head 45 degrees (when laying on face), turns to sound, follows objects past midline, social smile
Parent’s Little Baby: looks up to sound, smiles because he sees both his parents, one on either side of midline
4 months: lift head 90 degrees/raise up to chest, roll over, find midline, reach for objects, puts objects in mouth, coos (these are vowel sounds), and laughs
Fat Happy Baby: baby is rolling and laughing and cooing because he just discovered midline and is reaching for cake that he will cram into his mouth
6 months: sit up with no head lag, raking grasp, transfer objects between hands, babbles (consonants), recognizes familiar faces
Street-Corner Baby: sitting up on sidewalk, transferring a rake from hand to hand while babbling at people he thinks he recognizes
9 months: Crawl, pull to stand, point, specific babbling (mama, dada), stranger anxiety
Watch Dog Baby: crawls to window, pulls to stand to see out, points at stranger in yard and says “mama” to get attention of parents.
12 months: Walk, pincer grasp, 1 word, patacake, bye bye, peekaboo
Playful Zombie Baby: walking at you, snapping pincers, repeating one word over and over (brrraaaaains), and just wants to play patacake and peekaboo before waving bye bye.
15 months: walks well, imitates, controlled release of blocks (can stack 2)
Little Sister Baby: wants to be just like big sister, walks confidently to the blocks and imitates making a 2 block tower
18 months: Throw, scribble, 4 block tower, 1 step command, uses spoon/cup, points to parts of body
Sir Charming Baby: needs to get note to Rapunzel so scribbles note on paper to throw into high 4 block tower, catapult has cup on end, shoves note in with spoon, and throws note at tower, hitting Rapunzel in the face
2 years: Run, stairs (1 foot at a time), 20-50 words, 2 step command, parallel play
Bad Twins: mom gives two commands to twin boys to run to the stairs, then walk up the 25 stairs. Each walks up the 25 stairs not helping the other.
3 years: Jump, Tricycle, dresses self (shirt, pants, shoes), full name, “you, me, I”
James Bond Baby: springs into action … jumps into 3-piece suit, stands in front of mirror and says full name, jumps on tricycle. “You.Me. I,” is his pickup line.
4 years: Stairs (alternating feet), hop, undresses, 1 foot (4 seconds), 4 word phrases (complete sentences), cooperative play
Bedtime Story Baby: really wants story time, so runs up stairs, hops on one foot to undress, so she and mom can read a story together. A Wrinkle in Time.
5 years: Skip, Tie shoes, Difference between reality/fantasy
Oz Baby: ties ruby shoes, skips down Yellow Brick Road back to Kansas
Developmental assessment
Primitive reflexes
Mnemonic: MPRAG
M Moro
P Placing reflex
R Rooting
A Atonic neck reflex
G Grasp reflex
Head circumference with age
· Remember 3, 9, and multiples of 5:
Newborn 35 cm
3 mos 40 cm
9 mos 45 cm
3 yrs 50 cm
9 yrs 55cm
| |
| |
|
| |||||||||
| |||||||||
|
|
|
|
| |||||
|
|
|
|
| |||||
|
|
|
|
| |||||
Weights of children with age
Newborn 3 kg
6 mos 6 kg (2x birth wt at 6 mos)
1 yr 10 kg (3x birth wt at 1 yr)
3 yrs 15 kg (odd yrs, add 5 kg until 11 yrs)
5 yrs 20 kg
7 yrs 25 kg
9 yrs 30 kg
11 yrs 35 kg (add 10 kg thereafter)
13 yrs 45 kg
15 yrs 55 kg
17 yrs 65kg
124 124 rule.
1day birth wt (this is the easy one)
2week regain birth wt
4month 2x birth wt
12month 3x birth wt
24month 4x birth wt
If you want to change selection, open original toplevel document below and click on "Move attachment"
Summary
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Details
Discussion
Do you want to join discussion? Click here to log in or create user.