-
CARDIOLOGY
-
Down's + murmur, query VSD: name 3 things that would make you suspect it’s pathologic
-
Innocent: Sensitive (position, resp), Short, Single, Small (area), Soft, Sweet, Systolic
- Pathologic: loud (>3/6), harsh, pansystolic/diastolic/late systolic/conntinuous, cannot modify with position, abnormal exam, PHx congenital heart disease, RFs (high LSB, pansystolic/diastolic, radiates to back/neck, >II, harsh, click
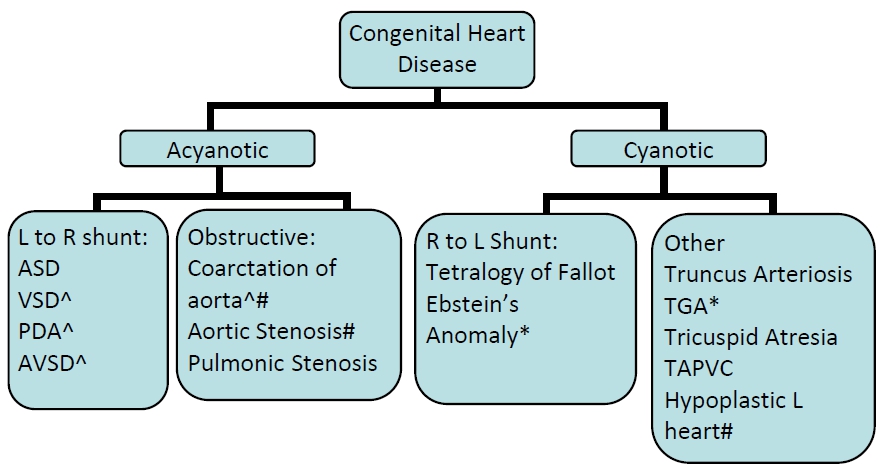
Congenital Heart Disease Functionally significant structural abnormalities of the heart and great vessels present at birth presented below.
Ebstein’s anomaly – opening of tricuspid valve is displaced towards the apex of the right ventricle = “atrialization” of the right ventricle. * CHD with cyanosis/tachypnea in first hours of life: TGA, Ebstein’s, Pulmonary atresia ^ CHD with CHF (excess pulm. flow): large VSD, AVSD, PDA, coarctation of the aorta # CHD with shock/catastrophy: critical coarctation or AS, interrupted aortic arch, Hypoplastic left heart5 most common types of Cyanotic Congenital Heart Defects (Five T’s)
• Tetralogy of Fallot (TOF): PA stenosis, RV hypertrophy, VSD,
overriding aorta
• Truncus arteriosus: A single trunk gives rise to the aortic arch,
pulmonary arteries and coronary arteries
• Transposition of Great Arteries (TGA): RV to aorta, LV to PA – the
pulmonary and systemic circulations are in parallel rather than in
series
• Tricuspid Atresia: Absence of the tricuspid valve forces all of the
systemic venous return across an ASD to mix with the pulmonary
venous return, often associated with pulmonary stenosis or atresia
• Total anomalous pulmonary venous connections (TAPVC): PV not
connected to LA
Note: Clinical presentations of these lesions usually differ markedly and may not
present with apparent cyanosis.
Defect in the formation of the intraventricular septum (varies in
size/location: muscular, perimembranous, or trabecular)
Clinical Findings
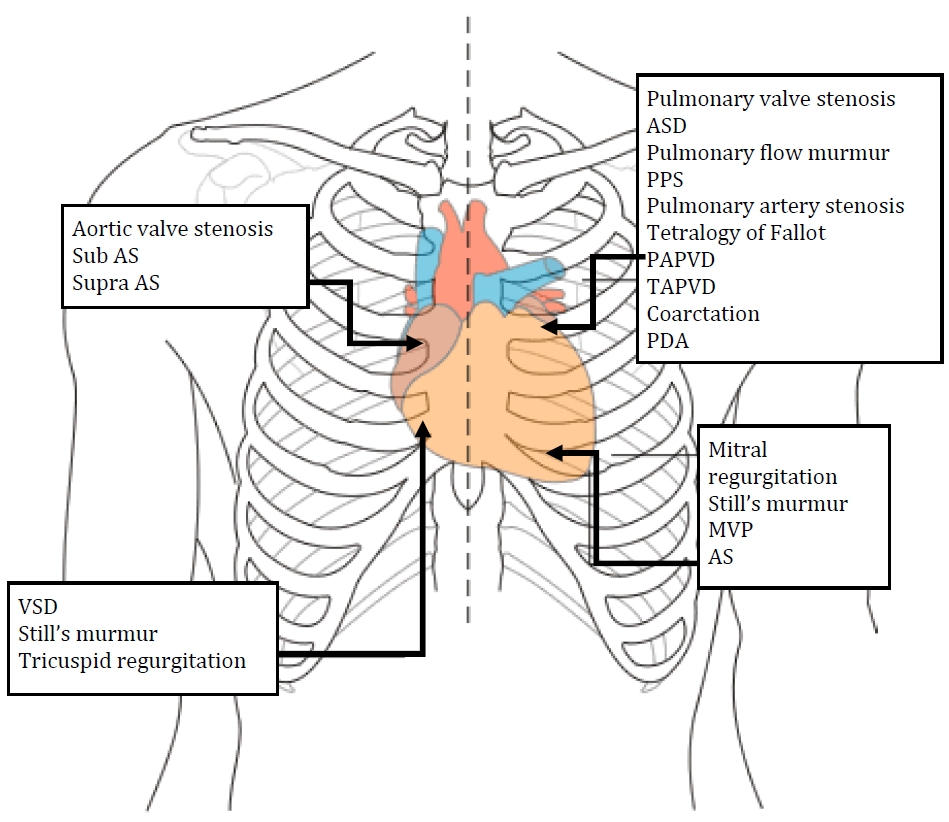
• Murmur: Holosystolic (soft or harsh):
o Soft murmur suggests the right sided pressures are high
o Harsh murmur suggests right sided pressures are relatively low
o Best heard at LLSB at >1 week old (when pulmonary vascular
resistance decreases enough for shunting LR)
• Heart sounds: loss of splitting of the second heart sound and a loud P2
suggests pulmonary hypertension
• CHF symptoms: respiratory distress, difficulty feeding (+diaphoresis),
FTT
Pathophysiology
Left to right shunt increased blood flow to lungs increased PV return
with LV overload and dysfunction, and later right heart dysfunction +/‐
pulmonary hypertension
Management
• For CHF symptoms: Diuretics and nutritional support
• If defect shows signs of closing, then monitor closely for any signs of
pulmonary hypertension
• Surgical correction of VSD if significant clinical symptoms not managed
medically (to avoid pulmonary vascular disease)
Atrial Septal Defect
Defect in the formation of the interatrial septum (varies in size/location:
ostium secundum, ostium primum, sinus venosus). Patent foramen ovale
does not ordinarily produce intracardiac shunts.
Clinical Findings
• Murmur: Systolic ejection murmur at pulmonic valve:
o Pressure gradient between atria is relatively small so shunt occurs
throughout cardiac cycle, the left‐to‐right shunt is silent.
o Murmur originates from pulmonary valve due to increased blood
flow producing a relative stenosis of the pulmonary valve (2‐3/6)
• Heart sounds: widely, fixed split S2
• CHF symptoms: Children rarely experience CHF even in the presence
of a large left to right shunt. CHF and pulmonary hypertension may
develop in the third and fourth decades of life.
Management
• Most children with ASD remain active and asymptomatic
• Depending on size (< 8 mm), spontaneous closure is likely
• Surgical closure if CHF does not respond to medical management or if
large left‐to‐right shunt
Patent Ducus Arteriosus
Persistent patency of normal fetal structure between the left pulmonary
artery and the descending aorta. More common in premature neonates.
Clinical Findings
• Murmur: Continuous murmur at the left infraclavicular area or upper
left sternal border
• Physical exam: Bounding peripheral pulses, hyperactive precordium,
tachycardia with or without a gallop rhythm, wide pulse pressure
Complications
• Children with small to medium PDA do well, typically do not need
intervention
• Children with large PDA can develop pulmonary vascular disease and
pulmonary hypertension (hemodynamics similar to patients with large
VSD)
Management
• In premature infants, short course of prostaglandin synthase inhibitors
(indomethacin, ibuprofen) administered
• If drug therapy unsuccessful or in adults and children, surgical closure
via ligation
Congestive Heart Failure
Occurs when the heart cannot deliver adequate cardiac output for the
metabolic needs of the body (CO=HR x SV)
Heart Failure may be secondary to:
• Low oxygen content (e.g., severe anemia)
• Hypermetabolic state (e.g., hyperthyroidism)
• High output circulatory state (‘overflow’)
• Abnormal myocardium (e.g., dilated cardiomyopathy)
Clinical Manifestations
Infants
• Tachypnea, tachycardia
• Failure to thrive, weak cry, irritability
• Hepatomegaly, cardiomegaly
• Gallop rhythm
Older Children
• Tachycardia
• Shortness of breath, fatigue, cough, wheeze
• Hepatomegaly, cardiomegaly
• High JVP, edema
• Gallop rhythm
2 Tachys:
‐ Tachycardia
‐ Tachypnea
2 Megalys:
‐ Cardiomegaly
‐ Hepatomegaly
Differential Diagnosis:
Preterm baby Anemia, PDA, large VSD, severely preterm, lung
disease
Infancy VSD, AVSD, left‐sided obstructive lesions (AS or
coarctation), myocarditis, AVM
Young child Left sided obstructive lesions, cardiomyopathy,
myocarditis, left‐to‐right shunt (e.g., VSD), AVM,
Kawasaki disease)
Older child Cardiomyopathy, myocarditis, left sided obstructive
lesions, endocarditis, Rheumatic heart disease, acute
hypertension, thyrotoxicosis, medications
Investigations/Imaging
• CXR
• ECG
• Echo
• Pre‐ and post‐ductal oxygen saturation
• Four limb blood pressure
o Systolic BP > 10 mmHg in upper body than lower body suggests
aortic arch pathology
Murmurs
Syllabus: Menashe V. Heart Murmurs. Pediatrics in Review. 2007;28(4):e19.
Description of murmurs
(1) Intensity (grade out of 6)
(2) Timing (systole/diastole)
(3) Quality (harsh, soft)
(4) Location
(5) Radiation
(6) Postural/positional manoeuvres that affect the murmur
Innocent vs. Pathological Murmurs
INNOCENT
Soft (Grade 1/6, 2/6)
Soft/blowing/vibratory
Systolic
Generally well localized
Varies with position/manoeuvre
PATHOLOGICAL
Loud (> Grade 3/6)
Harsh
Pansystolic, diastolic, late
systolic, continuous
Cannot modify with position
Timing /Sound of Pathologic Murmurs
• Pansystolic atrioventricular valve regurgitation, VSD, PDA
(continuous throughout systole and diastole and varies in intensityoften
described as machinery)
• Systolic ejection narrow semilunar valves or outflow tracts
• Early diastolic semilunar valve regurgitation
• Mid diastolic obstructed atrioventricular valves
• Newborn loud S2 (non‐split) pulmonary hypertension
Common Innocent Murmurs in Children
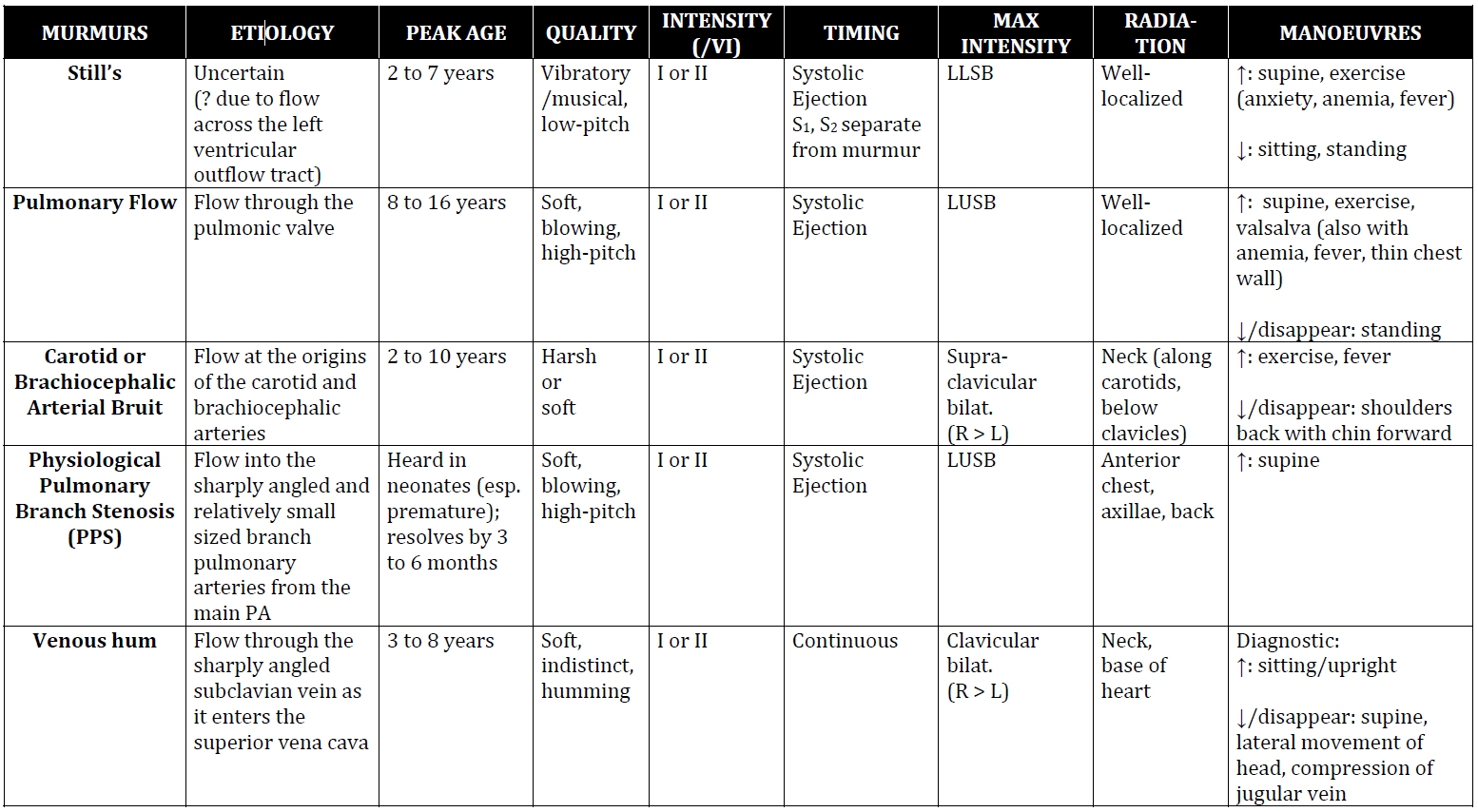
Summary
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |