Do you want BuboFlash to help you learning these things? Or do you want to add or correct something? Click here to log in or create user.
endo (day 8)
#has-images #ir #peds
-
ENDOCRINOLOGY
-
Diabetes mellitus
-
-
Best marker for insulin resistance?
-
MCQ: acanthosis nigricans
-
-
Puberty
-
-
13yo ♀, no onset of menarche. What questions would you ask on Hx (6)? What would you do O/E? When and how would you investigate?
-
Hx: Breast development, weight loss, pubic hair development, short stature, FHx, athlete, medical illness, high performance athlete
-
O/E: assess nutritional status, dysmorphism, evidence of chronic disease, signs of abuse or neglect, sexual development (“boobs→pubes→grow→flow”)
-
Ix (if no menarche >16 or pubertal >12): always (bone age, CBC/lytes, CRP, FSH/LH, EST/TEST, TSH/T4, IGF, U/A), consider (IBD panel, Celiac panel, etc.)
-
Precocious puberty in ♀: when are you worried and which tests would you order?
Hypoglycemia (Infants and Children)
Definition
Plasma glucose (PG) ≤2.8 mmol/L
Etiology
• Endocrine causes: Ketotic hypoglycemia, GH deficiency,
panhypopituitarism, ACTH deficiency, Addisons disease, excess
exogenous insulin
• Nonendocrine
causes: Sepsis/shock, liver disease, ingestion (e.g.
ethanol, salicylates, beta‐blockers), inborn error of metabolism
Clinical Presentation
• Autonomic symptoms: Sweating, weakness, tachycardia, tremor,
feelings of nervousness and/or hunger
• Neuroglycopenic symptoms: Lethargy, irritability, confusion, unusual
behaviour, hypothermia, seizure and coma
Investigations
Send critical labs (prior to initiating treatment) if PG ≤2.8 mmol/L:
Serum glucose, blood gas, electrolytes, insulin, GH, cortisol, free fatty acids,
ß‐hydroxybutyrate, acylcarnitines, total and free carnitine, serum amino
acids, NH4, lactate, urine organic acids, c‐peptide, urine sample for glucose,
ketones and reducing substances
Management
• Treat if PG <3.3 mmol/L and neurologic symptoms (confusion, seizure)
or PG ≤ 2.8 mmol/L
• Initial bolus of dextrose (5 mL/kg of D10W or 2 mL/kg of D25W),
then continuous dextrose infusion to maintain PG
• If no IV access, give glucagon IM or SC. Children <20 kg = 0.03 mg/kg,
max 0.5 mg/dose. Children >20 kg = 1 mg/dose. May repeat q20
minutes as needed
Diabetes Mellitus
Introduction
• Type 1 DM (DM1) accounts for 5‐10% of all diabetes
• Most commonly presents in childhood
o Age of onset has bimodal distribution: peaks at 4‐6 and 10‐14 yrs
o Family history a significant risk factor (5% for first‐degree
relatives)
• Incidence varies with geographical location
• Major Emergencies
o Diabetic ketoacidosis (DKA) ‐ initial presentation in 15‐67%
- Risk for DKA increases if age < 6 yrs or low SES
o Intercurrent illness
o Hypoglycemia
Pathophysiology
Genetic susceptibility + environmental trigger autoimmune β‐cell
destruction progressive insulin deficiency
Differential Diagnosis
• Type 2 Diabetes Mellitus (DM2)
o Disorder of insulin resistance
o Typically presents after puberty
o Associated symptoms: metabolic syndrome, obesity, PCOS,
acanthosis nigracans
• Genetic defects in β‐cell function
• Medications: atypical anti‐psychotics, immunosuppressants
(cyclosporine, tacrolimus), glucocorticoids, chemotherapeutics
• Diseases of exocrine pancreas: cystic fibrosis, chronic pancreatitis
Risk Factors
• Risk increases if family history of DM1 (5% for first‐degree relatives)
• Bimodal age of presentation with peaks between 4‐6 yrs and 10‐14 yrs
• DKA ‐ more likely if <6 yrs or low SES
History
• Polyuria, polydipsia, weight loss, polyphagia, nocturia, enuresis, recent
infection, vomiting, abdominal pain, confusion/lethargy
• Family history of DM1 or DM2, autoimmune conditions (e.g., thyroid,
celiac or Addison disease, vitiligo)
Physical Exam
• Vital signs
• Signs of dehydration
• Lethargy/drowsiness
• Kussmaul’s respiration (rapid, deep, sighing)
• Ketones on breath (fruity breath odour)
Investigations
• Diagnosis of DM1:
o HbA1C ≥6.5% OR
o fasting plasma glucose (PG) ≥7 mmol/L OR
o 2 hour PG in 75 g OGTT ≥11.1 mmol/L OR
o random PG ≥11.1 mmol/L with classic symptoms of hyperglycemia
• Urinalysis for glucose and ketones
• If concern about DKA
o Venous or arterial blood gas, osmolality*, PG, HbA1C, Na**, K, Cl,
Mg, Phos, Ca, bicarbonate, urea, creatinine, CBC, differential,
cultures if evidence of infection
• Anti‐GAD, anti‐islet, insulin antibodies if diagnosis not clear
*Effective osmolality = 2 x (Na + K) + glucose
**Corrected Na = measured Na + 0.3 x (plasma glucose – 5.5) mmol/L
Initial Management
• DKA
o Admission to ICU or ward
o For ER management, refer to
www.health.gov.on.ca/english/providers/pub/diabetes/child_post
er.pdf
• Non‐DKA
o Initiate initial daily insulin dose of 0.4‐0.6 units/kg/day
o 2/3 given in am: 1/3 as rapid acting (Humalog or Novorapid), 2/3
as intermediate‐acting (Humulin N or Novolin N)
o 1/3 given in pm: 1/3 as rapid acting, 2/3 as intermediate‐acting
o Accu‐cheks before each meal and at bedtime
o Discharge from emergency department with immediate outpatient
management by multi‐disciplinary diabetes team
INSULIN TYPE ONSET PEAK DURATION
Rapid acting:
Lispro (Humalog)
Aspart (Novorapid)
10‐15
min 1‐2h
1‐1.5 h
3.5‐4.75h
3‐5 h
Short acting:
Humulin‐R
Novolin Toronto
30 min 2‐3 h 6.5h
Intermediate acting
NPH (Humulin N, Novolin N) 1‐3 h 5‐8 h Up to 18h
Long acting:
Detemir (Levemir)
Glargine (Lantus)
90 min
N/A 16‐24 h
24 h
Longterm Management
• Comprehensive, multidisciplinary visits every 3 months
• Intercurrent illness: Check PG and ketones q4hrs, do not stop insulin,
may need to adjust insulin dose, ensure fluid intake, ER if vomiting and
not tolerating fluids
• Hypoglycemia: Treat PG <4 mmol/L with 10‐15 g of carbohydrate
(CHO) (e.g., 125 mL of juice, 2‐3 dextrose tablets), wait 10‐15 minutes,
recheck blood glucose, repeat with 10‐15 g of CHO if PG remains <4
mmol/L. If next meal is >1 hr away, consume snack with 15 g CHO and
protein source.
RECOMMENDED GLYCEMIC TARGETS IN TYPE I DM
Age (years) HbA1C (%) Fasting/preprandial PG (mmol/L)
<6 <8 610
612
<7.5 410
1318
≤7 47
Complications
• Diabetes (DM1 and DM2)
o Microvascular: retinopathy, nephropathy, neuropathy
o Macrovascular: cardiovascular, cerebrovascular, peripheral
vascular
• During DKA Cerebral edema occurs in 1% of children
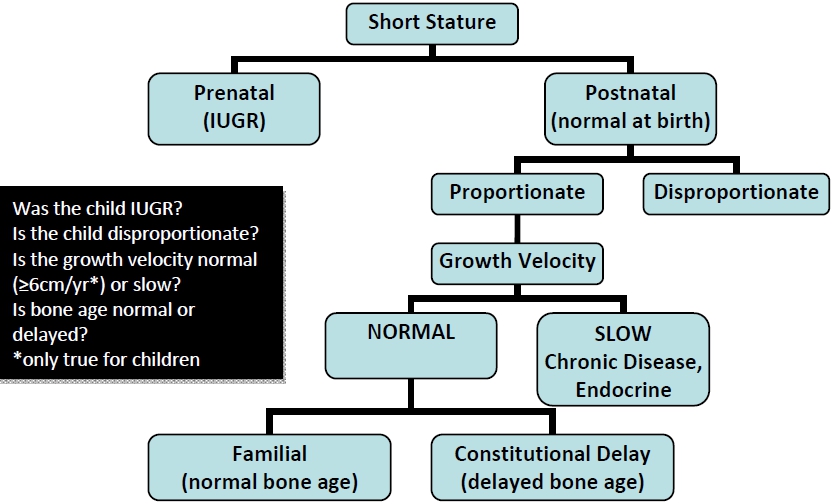
Short Stature
Definition
• Ht <3rd% OR height crossing major percentile lines OR low growth
velocity (<25th%)
Differential Diagnosis
• Alone (neglected infant)
• Bone dysplasia (rickets, achondroplasia)
• Chromosomal (Turners, T21)
• Delayed Growth (constitutional delay)
• Endocrine (hypopituitary, GH def, hypothyroid, Cushing)
• Familial
• GI malabsorption (celiac, Crohns)
NonPathological
Short Stature Normal
Growth Velocity
• Constitutional Delay of Growth and Puberty:
o Normal growth velocity during childhood years with height below
but parallel to 3rd %
o Delayed bone age and pubertal maturation
o Attainment of normal or near‐normal adult height
o FHx of delayed puberty but normal mid‐parental height
o May require short term therapy with androgens (males)
• Familial Short Stature:
o Normal bone age
o Normal growth velocity below but parallel normal growth curves
o Normal onset of puberty
o FHx of short stature
o Treatment not indicated
• Syndromic
o Special growth charts are available for Turner Syndrome,
Achondroplasia (typically grow along %iles specific to their
condition ‐ normal growth velocity)
Pathological Short Stature Decreased
Growth Velocity:
• Primordial (height, weight, head circumference affected)
• Chromosomal: e.g., Turner, T21, dysmorphic features
• Skeletal dysplasias
• IUGR (teratogen, placental insufficiency, infection)
• Endocrine (height affected more than weight ‐ “short and fat”)
o GH deficiency‐ (rare) slow growth velocity, decreased bone age
o Hypothyroidism
o Hypercortisolism ‐ exogenous or endogenous
o Hypopituitarism
o Hypogonadism: delayed puberty
• Chronic Disease (weight affected more than height ‐ “short and
skinny”)
o Cyanotic congenital heart disease
o Malnutrition: macronutrient, mineral, neglect
o Malabsorption: celiac, IBD, cystic fibrosis
o Chronic infections
o Chronic illnesses (e.g. chronic renal failure)
• Psychosocial neglect (Usually decreased weight, height and HC if
severe)
o ‘Psychosocial dwarfism’
History
• Pregnancy and birth history
• Birth measurements, growth pattern
• Developmental history
• Nutrition history
• Pubertal development
• Illnesses and infections
• Headaches, vision changes, and stigmata of endocrine imbalances
• Family relationships
• Familial patterns of height, weight, growth, puberty
Physical Exam
• Ht/Wt/HC‐ plot on growth chart
o Obtain old growth charts
o Decreased growth velocity may be more worrisome than actual
height
• HR, RR, BP
• Arm span or upper to lower (U/L) segment ratio*
• Systemic changes secondary to endocrine/pituitary condition (optic
fundi, visual fields secondary to pituitary compression)
• Sexual development staging
• Nutritional status, dysmorphism, evidence of chronic disease, signs of
abuse or neglect
*Upper to lower segment ratio (U/L)
• Landmark for lower segment ‐ pubic symphysis
• Standard U/L segment ratio:
o Newborn: 1.7
o 4 year old child: 1.4
o Adult: 0.9 (male); 1.0 (female)
• Ratio increased in skeletal dysplasias affecting spine or long bones
(Achondroplasia), hypothyroidism
Investigations/Imaging
• Determine Mid‐Parental Height* (expected adult height)
o Boy = (Father ht (cm) + Mother ht (cm) + 13cm) / 2
o Girl = (Father ht (cm) + Mother ht (cm) ‐ 13cm) / 2
• Bone age (AP x‐ray of L hand and wrist)
• Endocrine: TSH, T4, GH stimulation test
• Chronic illness: lytes, Cr, BUN, LFT, Ca, IgG/IgM/IgA, ESR, urinalysis
• Malabsorption: fecal fat, albumin, ferritin, celiac screen, sweat chloride
• Consider karyotype to rule out Turners in females or if dysmorphic
features are present
Diagnostic Approach
Management
• Depends on severity of problem as perceived by parents, child
• Typically no treatment if non‐pathological
• GH therapy if requirements are met
o GH deficient on 2 different stimulation tests
o Ht<<3%ile or growth velocity <3%ile
o Delayed bone age
o Patient has Turners, Noonan or chronic renal failure
• Consider: testosterone/estrogen (in pubertal delay); GnRH agonists,
aromatase inhibitors (to delay puberty and epiphyseal fusion)
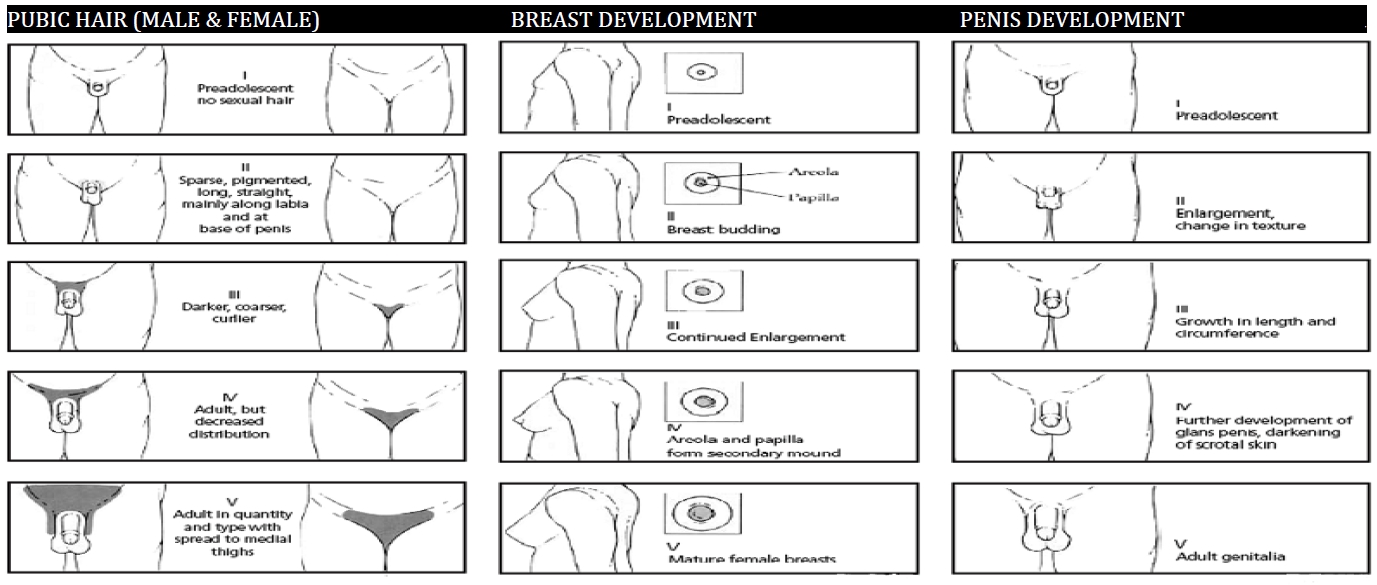
Puberty and Tanner Staging
Puberty
Female (normal onset: ages 7‐13 – earlier in African Americans)
• Breast development pubarche growth spurt menarche
• Early puberty common but not as worrisome (most are constitutional),
late puberty rare but worrisome (often organic)
Male (normal onset: ages 9‐14)
• Testicular enlargement pubarche peak growth spurt
• Voice change not reliable
• Early puberty uncommon but worrisome (~50% are organic), late
puberty common and not as worrisome (most are constitutional)
General History
• Symptoms of puberty
• General growth, developmental, and nutritional history
• Family history of pubertal onset
• General health, past and current illnesses
• Headaches, seizures, abdominal complaints
General Physical Exam
• Growth parameters, velocity
• Stigmata of endocrinopathies including hursutism, virilization
• Sexual maturity rating (Tanner Staging)
Sexual Maturity Rating (Tanner Staging)
Precocious Puberty
Definition
Secondary sexual development: <8 years in girls, <9 years in boys (more
common and usually idiopathic in girls, more pathological in boys)
Isosexual vs. contrasexual precocity:
• Isosexual: phenotypically appropriate secondary sexual characteristics
• Contrasexual: development of secondary sexual characteristics
opposite to genotypic sex, order of development different than regular
puberty (e.g., virilizing tumor (ovarian, adrenal), CAH, exogenous
androgen exposure)
Complications
• Decreased adult height (premature epiphyseal closure)
• Adverse psychosocial outcomes, such as early high‐risk social
behaviour, higher risk of abuse
Etiology
Central (GnRH dependent) Hypergonadotropic
Hypergonadism
• Bone age advancement + growth acceleration + 2° sex characteristics
• ↑LH/FSH + ↑testosterone/estrodiol (as in normal puberty)
• Premature activation of HPG axis
• More common in females (9:1)
• Most common initial signs: breast (female); testicular enlargement
(male)
• Differential Diagnosis
o Idiopathic: premature activation of HPG axis (most common cause
in girls)
o Obesity
o CNS: cysts, tumors, head trauma, encephalitis, meningitis,
hydrocephalus, increased ICP, irradiation
o Primary hypothyroidism (Van Wyk‐Grumbach syndrome)
o NF, primary severe hypothyroidism
Peripheral (GnRH Independent) Hypogonadotropic
Hypergonadism
• ↓LH/FSH + ↑testosterone/estrodiol
• Differential Diagnosis
o Adrenal disorders: CAH, adrenal neoplasm (contrasexual precocity)
o Ovarian cysts, granulosa cell tumors (estrogen‐secreting)
o Theca cell and Leydig cell tumors (testosterone‐secreting)
o Germ cell tumors such as hepatoblastoma, teratoma, germinoma
(gonadotropin/hCG‐secreting)
o Endogenous steroids
o McCune‐Albright syndrome
o Hypothyroidism‐ Van Wyk and Grumbach Syndrome
o Aromatase Excess Syndrome
History
• Symptoms of puberty
• Family history of puberty onset
• Medical illness
Physical Exam
• Growth velocity‐minimum 4cm/yr
• Tanner staging
• Complete physical exam including neurological exam
Investigations/Imaging
ALWAYS DO CONSIDER
Bone Age
LH, FSH
Estradiol, Testosterone
DHEA‐S
17‐hydroxyprogresterone
TSH, T4
Pelvic U/S
MRI head
β‐hCG
GnRH or Leuprolide stimulation
test
ACTH stimulation test
Management
Central (GnRH dependent) Hypergonadotropic
Hypergonadism
• Goal of therapy
o Preserve adult height
o Alleviate psychosocial effects
• Pharmacotherapy: GnRH agonists (i.e. leuprolide)
o downregulate HPG axis when administered continuously
o most effective at delaying central precocious puberty
Peripheral (GnRH Independent) Hypogonadotropic
Hypergonadism
• Goal of therapy:
o Treat underlying pathology
o Limit effects of elevated sex steroids
• Pharmacotherapy: ketoconazole (androgen‐synthesis inhibitor),
spironolactone (steroid receptor blocker), tamoxifen (SERM),
anastrozole, letrozole (aromatase inhibitor)
Indications for medical intervention to delay progression of puberty
• Male
• Bone age advancing more quickly than height age
• Age <6
• Psychological issues
Delayed Puberty
Definition
• Absence of pubertal development by age 13 in girls and age 14 in boys
(more common and usually idiopathic in boys, more suggestive of
pathology in girls), or
• Absence of menarche by 16 or within 5 years of pubertal onset
Etiology
Central Causes – Hypogonadotropic hypogonadism
• Delay in activation of H‐P‐G axis
• ↓ LH/FSH + ↓ testosterone/estrodiol
• Delayed bone age
• Differential Diagnosis
o Idiopathic: Constutional Delay of Growth and Puberty (most
common cause in boys)
o Systemic illnesses
o Endocrinopathies (hypopituitarism, GH, thyroid, prolactin,
cortisol, DM)
o Excessive exercise, anorexia nervosa, malnutrition
o CNS infiltrative diseases, CNS infection, irradiation, trauma
o Genetic conditions, e.g. Kallman Syndrome
Peripheral Causes – Hypergonadotropic hypogonadism
• Primary gonadal failure
• ↑ LH/FSH + ↓ testosterone/estradiol
• Differential Diagnosis
o Genetic syndromes: Turner, Klinefleter, Noonan
o Gonadal damage: infection, trauma, testicular torsion, radiation,
chemotherapy
o Gonadal Dysgenesis, cryptorchidism
o Hormonal: androgen insensitivity, 5‐alpha‐reductase deficiency
History
• Weight loss/nutritional status?
• Short stature?
• Family history of pubertal onset?
• Medical illness or previous treatments?
• History of celiac disease, thyroid disease, anorexia, IBD?
• Psychosocial functioning
Physical Exam
• Growth velocity ‐ minimum 4cm/yr
• Tanner staging (testicular volume > 3 mL indicates puberty)
• Neurological exam
Investigations/Imaging
ALWAYS DO CONSIDER
Bone age
CBC, lytes, renal & liver function
ESR, CRP
FSH, LH, Testosterone, Estradiol
TSH, T4
IGF‐1, IGFBP‐3
Urinalysis
IBD panel
Celiac Panel
Prolactin
Karyotype
Head MRI
Pelvic U/S
LH levels following GnRH
stimulation test
Management
• Identify and treat underlying cause
• Hormone replacement: cyclic estradiol & progesterone (females);
testosterone (males)
o dosing regimen aimed at mimicking normal pubertal development
• Counseling for depression, anxiety, and low self esteem that may arise
If you want to change selection, open original toplevel document below and click on "Move attachment"
Summary
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Details
Discussion
Do you want to join discussion? Click here to log in or create user.