ACS
#has-images
Acute coronary syndrome (ACS) is an umbrella term covering a number of acute presentations of ischaemic heart disease.
It covers a number of presentations, including
- ST elevation myocardial infarction (STEMI)
- non-ST elevation myocardial infarction (NSTEMI)
- unstable angina
Before we go into more detail into these presentations it's useful to take a step back and consider how such conditions develop.
ACS generally develops in patients who have ischaemic heart disease, either known or previously undetected. Ischaemic heart disease is a term synonymous with coronary heart disease and coronary artery disease. It describes the gradually build up of fatty plaques within the walls of the coronary arteries. This leads to two main problems:
- 1. Gradual narrowing, resulting in less blood and therefore oxygen reaching the myocardium at times of increased demand. This results in angina, i.e. chest pain due to insufficient oxygen reaching the myocardium during exertion
- 2. The risk of sudden plaque rupture. The fatty plaques which have built up in the endothelium may rupture leading to sudden occlusion of the artery. This can result in no blood/oxygen reaching the area of myocardium.
Remember that there are a large number of factors which can increase the chance of a patient developing ischaemic heart disease:
| Unmodifiable risk factors | Modifiable risk factors |
|---|---|
| Increasing age Male gender Family history | Smoking Diabetes mellitus Hypertension Hypercholesterolaemia Obesity |
Pathophysiology
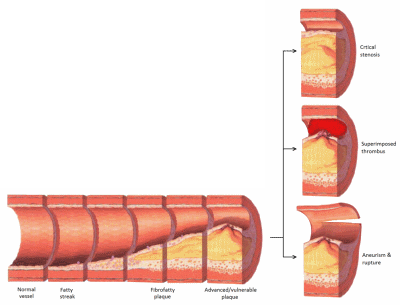
Ischaemic heart disease is a complex process which develops over a number of years. A number of changes can be seen:
- initial endothelial dysfunction is triggered by a number of factors such as smoking, hypertension and hyperglycaemia
- this results in a number of changes to the endothelium including pro-inflammatory, pro-oxidant, proliferative and reduced nitric oxide bioavailability
- fatty infiltration of the subendothelial space by low-density lipoprotein (LDL) particles
- monocytes migrate from the blood and differentiate into macrophages. These macrophages then phagocytose oxidized LDL, slowly turning into large 'foam cells'. As these macrophages die the result can further propagate the inflammatory process.
- smooth muscle proliferation and migration from the tunica media into the intima results in formation of a fibrous capsule covering the fatty plaque.
 | |
| Image sourced from Wikipedia |  |
Diagram showing the progression of atherosclerosis in the coronary arteries with associated complications on the right.
 | |
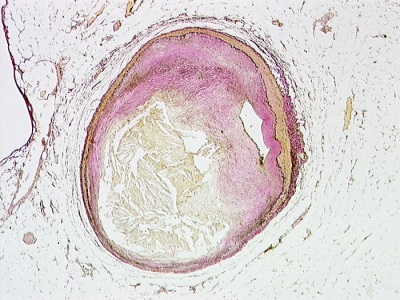
| Image sourced from Wikipedia |  |
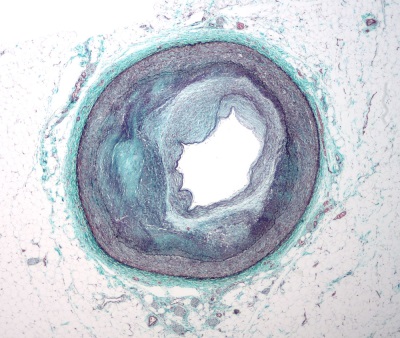
Slide showing a markedly narrowed coronary artery secondary to atherosclerosis. Stained with Masson's trichrome.
Complications of atherosclerosis
Once a plaque has formed a number of complications can develop:
- the plaque forms a physical blockage in the lumen of the coronary artery. This may cause reduced blood flow and hence oxygen to the myocardium, particularly at times of increased demand, resulting clinically in angina
- the plaque may rupture, potentially causing a complete occlusion of the coronary artery. This may result in a myocardial infarction
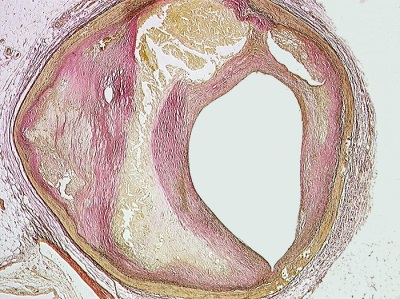
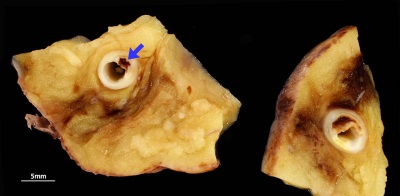 | |
| © Image used on license from PathoPic |  |
Ruptured coronary artery plaque resulting in thrombosis and associated myocardial infarction.
 | |
| © Image used on license from PathoPic |  |
Pathological specimen showing infarction of the anteroseptal and lateral wall of the left ventricle. There is a background of biventricular myocardial hypertrophy.
Symptoms and signs
The classic and most common feature of ACS is chest pain.
- typically central/left-sided
- may radiate to the jaw or the left arm
- often described as 'heavy' or constricting, 'like an elephant on my chest'
- it should be noted however in real clinical practice patients present with a wide variety of types of chest pain and patients/doctors may confuse ischaemic pain for other causes such as dyspepsia
- certain patients e.g. diabetics/elderly may not experience any chest pain
Other symptoms in ACS include
- dyspnoea
- sweating
- nausea and vomiting
Patients presenting with ACS often have very few physical signs to ellicit:
- pulse, blood pressure, temperature and oxygen saturations are often normal or only mildly altered e.g. tachycardia
- if complications of the ACS have developed e.g. cardiac failure then clearly there may a number of findings
- the patient may appear pale and clammy
Investigations
The two most important investigations when assessing a patient with chest pain are:
- ECG
- cardiac markers e.g. troponin
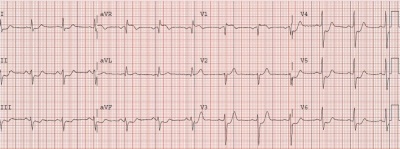
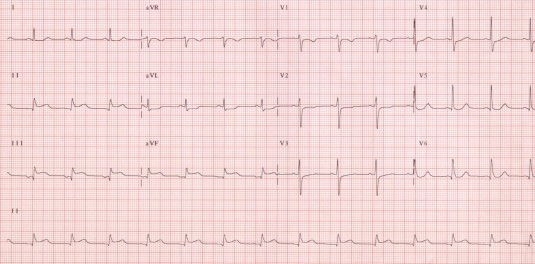 | |
ECG showing a ST elevation myocardial infarction (STEMI). Note by how looking at which leads are affected (in this case II, III and aVF) we are able to tell which coronary arteries are blocked (the right coronary artery in this case). A blockage of the left anterior descending (LAD) artery would cause elevation of V1-V4, what is often termed an 'anterior' myocardial infarction.
 | |
| © Image used on license from Dr Smith, University of Minnesota |   |
ECG showing a non-ST elevation myocardial infarction (NSTEMI). On the ECG there is deep ST depression in I-III, aVF, and V3-V6. aVR also has ST elevation. Deep and widespread ST depression is associated with very high mortality because it signifies severe ischemia usually of LAD or left main stem.
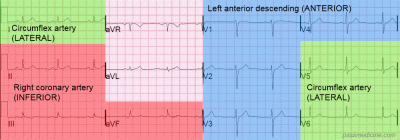
The table below shows a simplified correlation between ECG changes and coronary territories:
| ECG changes | Coronary artery | |
|---|---|---|
| Anterior | V1-V4 | Left anterior descending |
| Inferior | II, III, aVF | Right coronary |
| Lateral | I, V5-6 | Left circumflex |
 | |
 | |
Diagram showing the correlation between ECG changes and coronary territories in acute coronary syndrome
Management
Once a diagnosis of ACS has been made there are a number of elements to treatment:
- prevent worsening of presentation (i.e. further occlusion of coronary vessel)
- revascularise (i.e. 'unblock') the vessel if occluded (patients presenting with a STEMI)
- treat pain
A commonly taught mnemonic for the treatment of ACS is MONA:
- Morphine
- Oxygen
- Nitrates
- Aspirin
Whilst useful it should be remember that not all patients require oxygen therapy. British Thoracic Society guidelines are now widely adopted and oxygen should only be given if the oxygen saturations are < 94%.
For patients who've had a STEMI (i.e. one of the coronary arteries has become occluded) the priority of management is to reopen, or revascularise, the blocked vessel.
- a second antiplatelet drug should be given in addition to aspirin. Options include clopidogrel, prasugrel and ticagrelor
- for many years the treatment of choice was thrombolysis. This involved the intravenous administration of a thrombolytic or 'clot-busting' drug to breakdown the thrombus blocking the coronary artery
- since the early 2000's thrombolysis has been superseded by percutaneous coronary intervention (PCI). In this procedure the blocked arteries are opened up using a balloon (angioplasty) following which a stent may be deployed to prevent the artery occluding again in the future. This is done via a catheter inserted into either the radial or femoral artery
If a patient presents with an NSTEMI then a risk stratification too (such as GRACE) is used to decide upon further management. If a patient is considered high-risk or is clinically unstable then coronary angiography will be performed during the admission. Lower risk patients may have a coronary angiogram at a later date.
Secondary prevention
Patients who've had an ACS require lifelong drug therapy to help reduce the risk of a further event. Standard therapy comprises the following as a minimum:
- aspirin
- a second antiplatelet if appropriate (e.g. clopidogrel)
- a beta-blocker
- an ACE inhibitor
- a statin
Further images
The following images show the progress of coronary artery atherosclerosis:
 | |
| © Image used on license from PathoPic |  |
Normal coronary artery with blood in the lumen.
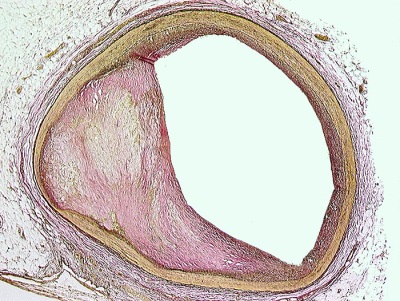 | |
| © Image used on license from PathoPic |  |
Slightly stenosed coronary artery
 | |
| © Image used on license from PathoPic |  |
Moderately stenosed coronary artery, beetween 50-75%
 | |
| © Image used on license from PathoPic |  |
Severely stenosed coronary artery
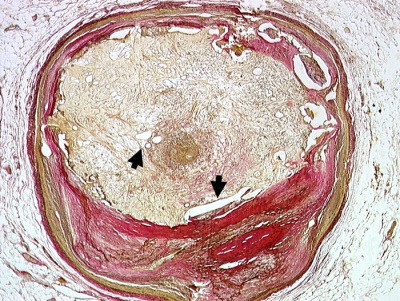 | |
| © Image used on license from PathoPic |  |
Recanalised old atherothrombotic occlusion of a coronary artery. Numerous small neolumina recanalising the organised occluding thrombus (indicated with arrows)