Edited, memorised or added to reading queue
on 14-Dec-2023 (Thu)
Do you want BuboFlash to help you learning these things? Click here to log in or create user.
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Flashcard 7604747242764
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Open it
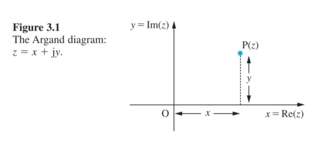
The angle between the positive real axis and OP is called the argument of \(z\), which is usually denoted by \(\arg{z}\): \(\displaystyle \arg z=\angle z=\theta, \text{where }\tan{\theta}=\frac{y}{x},z\neq 0\)
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Flashcard 7604752223500
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
复数向量所在区间与其幅角的关系
复数向量所在区间与其幅角的关系:\(\theta=\tan^{-1}\left(\frac{y}{x}\right)= \begin{cases}\tan^{-1}\left(\frac{y}{x}\right) & \text { if } x>0 \\\pi-\tan^{-1}\left(\frac{y}{-x}\right) & \text { if } x<0 \text { and } y \geq 0 \\-\left(\pi-\tan^{-1}\left(\frac{y}{x}\right)\right) & \text { if } x<0 \text { and } y<0 \\ +\frac{\pi}{2} & \text { if } x=0 \text { and } y>0 \\ -\frac{\pi}{2} & \text { if } x=0 \text { and } y<0 \\ \text { undefined } & \text { if } x=0 \text { and } y=0\end{cases}\)
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
h postdischarge readmission rates [1-12]. The onset and severity of symptoms of ADHF vary and depend on the nature of the underlying cardiac disease and the rate at which the syndrome develops. <span>The largest proportion of patients (70 percent) with ADHF are admitted due to worsening chronic HF, up to 15 to 20 percent of patients present with HF for the first time, and approximately 5 percent are admitted for advanced or end-stage HF. Low blood pressure (<8 percent) or shock (<3 percent) are complications of ADHF [1,2,11]. CAUSES AND PRECIPITATING FACTORS — Appropriate therapy for ADHF requires identification
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
with ADHF are admitted due to worsening chronic HF, up to 15 to 20 percent of patients present with HF for the first time, and approximately 5 percent are admitted for advanced or end-stage HF. <span>Low blood pressure (<8 percent) or shock (<3 percent) are complications of ADHF [1,2,11]. CAUSES AND PRECIPITATING FACTORS — Appropriate therapy for ADHF requires identification of the specific HF phenotype as well as the potential causes and precipitants. Causes are the pr
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
oximately 5 percent are admitted for advanced or end-stage HF. Low blood pressure (<8 percent) or shock (<3 percent) are complications of ADHF [1,2,11]. CAUSES AND PRECIPITATING FACTORS — <span>Appropriate therapy for ADHF requires identification of the specific HF phenotype as well as the potential causes and precipitants. Causes are the primary condition or disease process leading to the development of HF. Precipitants are triggers or contributing factors for decompensation in patients with established c
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
e primary condition or disease process leading to the development of HF. Precipitants are triggers or contributing factors for decompensation in patients with established chronic heart disease. <span>The following are the major causes for new onset ADHF: ●Coronary artery disease: •Acute coronary syndrome. (See "Initial evaluation and management of suspected acute coronary syndrome (myocardial infarction, unstable angina) in the emergency department" and "Diagnosis of acute myocardial infarction".) -Myocardial infarction (MI)/ischemia. -Ventricular septal rupture. (See "Acute myocardial infarction: Mechanical complications".) ●Arrhythmias: •Atrial fibrillation and atrial flutter. (See "Overview of the acute management of tachyarrhythmias", section on 'Narrow QRS complex tachyarrhythmias'.) •Ventricular tachycardia, ventricular fibrillation, or high-frequency ventricular ectopy. (See "Overview of the acute management of tachyarrhythmias", section on 'Wide QRS complex tachyarrhythmias'.) ●Myocarditis. (See "Clinical manifestations and diagnosis of myocarditis in adults".) ●Acute valve syndromes: •Acute mitral or aortic regurgitation secondary to infective endocarditis, ruptured chordae of a degenerative mitral valve, ischemic papillary muscle rupture, or aortic dissection. (See "Acute mitral regurgitation in adults" and "Acute aortic regurgitation in adults".) •Thrombosed mechanical aortic or mitral valve. (See "Bioprosthetic valve thrombosis, thromboembolism, and obstruction: Clinical manifestations and diagnosis".) •Tear or perforation of a bioprosthetic aortic or mitral valve leaflet. (See "Clinical manifestations and diagnosis of surgical aortic and mitral prosthetic valve regurgitation".) ●Progressive valve disease: •Severe aortic or mitral valve stenosis, including left atrial myxoma. (See "Clinical manifestations and diagnosis of aortic stenosis in adults" and "Rheumatic mitral stenosis: Clinical manifestations and diagnosis".) •Severe aortic or mitral regurgitation. (See "Clinical manifestations and diagnosis of chronic aortic regurgitation in adults" and "Clinical manifestations and diagnosis of chronic mitral regurgitation".) ●Cardiomyopathic states: •Hypertrophic cardiomyopathy. (See "Hypertrophic cardiomyopathy: Clinical manifestations, diagnosis, and evaluation".) •Recent onset dilated cardiomyopathy. (See "Familial dilated cardiomyopathy: Prevalence, diagnosis and treatment" and "Causes of dilated cardiomyopathy".) •Tachycardia mediated cardiomyopathy. (See "Arrhythmia-induced cardiomyopathy".) •Stress (takotsubo) cardiomyopathy. (See "Clinical manifestations and diagnosis of stress (takotsubo) cardiomyopathy".) ●Poorly controlled hypertension: •Bilateral renal artery stenosis. (See "Chronic kidney disease resulting from atherosclerotic renal artery stenosis", section on 'Clinical manifestations'.) ADHF due to decompensation of chronic HF can occur without known precipitant factors but more often occurs with one or more factors, such as infection, uncontrolled hypertension, rhythm
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
".) ●Poorly controlled hypertension: •Bilateral renal artery stenosis. (See "Chronic kidney disease resulting from atherosclerotic renal artery stenosis", section on 'Clinical manifestations'.) <span>ADHF due to decompensation of chronic HF can occur without known precipitant factors but more often occurs with one or more factors, such as infection, uncontrolled hypertension, rhythm disturbances, and nonadherence with drugs and diet. Moreover, the in-hospital course is determined by the interplay between precipitants, underlying structural heart disease, and comorbidities. These factors are listed in the table (tabl
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
le Access Help & Training Demos Wolters Kluwer Health Emmi® Facts & Comparisons® Lexicomp® Medi-Span® Loading Please wait 1 of 11 Export to Powerpoint Print Share Bookmark Rate Feedback <span>Precipitants of heart failure Dietary indiscretion Vigorous fluid administration Noncompliance to medical regimen Worsening renal failure Uncontrolled hypertension Anemia Systemic infection Pulmonary embolism Myocardial ischemia Tachyarrhythmias and bradyarrhythmias Electrolyte disturbances Severe emotional or physical stress Hyperthyroidism and hypothyroidism Cardiodepressant and other drugs Anti-inflammatory drugs Antiarrhythmic drugs Calcium channel blockers Beta adrenergic blocking agents Graphic 117289 Version 1.0 © 2023 UpToDate, Inc. and/or its affiliates. All Rights Reserved. Graphics in this topic Precipitants of heart failure Acute decompensated heart failure: Rapi
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
al course is determined by the interplay between precipitants, underlying structural heart disease, and comorbidities. These factors are listed in the table (table 1). CLINICAL MANIFESTATIONS — <span>Patients present with a myriad of chief complaints, symptoms, and physical examination findings. Such heterogeneity prompts an initially broad differential diagnosis, thus securing the correct diagnosis can be challenging. For practical purposes, it is helpful to view the presentation of ADHF according to the predominant clinical characteristics on admission. As noted above, most patients presenting with
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
ened over the preceding days and weeks but have not been sufficient for the patient to seek medical attention. In a minority of patients, an episode of ADHF may be the first presentation of HF. <span>Approximately 50 percent of patients hospitalized for HF have HF with preserved ejection fraction (HFpEF; left ventricular ejection fraction [LVEF] >50 percent); the remainder of patients have HF with reduced ejection fraction (HFrEF; LVEF ≤40 percent) or HF with mid-range ejection fraction (LVEF 41 to 50 percent). (See "Epidemiology of heart failure", section on 'Magnitude of the problem'.) The following five clinical and hemodynamic profiles are modified from those described in the 2021 European
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
reduced ejection fraction (HFrEF; LVEF ≤40 percent) or HF with mid-range ejection fraction (LVEF 41 to 50 percent). (See "Epidemiology of heart failure", section on 'Magnitude of the problem'.) <span>The following five clinical and hemodynamic profiles are modified from those described in the 2021 European Society of Cardiology guidelines for the diagnosis and treatment of ADHF [12]: ●ADHF without pulmonary edema ●ADHF with severe pulmonary edema ●Cardiogenic shock ●High-output HF ●Right HF The above clinical groups are not mutually exclusive (eg, a patient with hypertensive crisis or cardiogenic shock may develop severe pulmonary edema). ADHF — This syndrome is seen in patients with new-onset HF or acute decompensation of chronic HF who develop signs or symptoms of decompensation; in this setting, there is no cardiogeni
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
ardiogenic shock ●High-output HF ●Right HF The above clinical groups are not mutually exclusive (eg, a patient with hypertensive crisis or cardiogenic shock may develop severe pulmonary edema). <span>ADHF — This syndrome is seen in patients with new-onset HF or acute decompensation of chronic HF who develop signs or symptoms of decompensation; in this setting, there is no cardiogenic shock or hypertensive crisis. There may be no, or mild, pulmonary congestion. This scenario accounts for 50 to 70 percent of all HF admissions [13-16]. In contrast to the other phenotypes, this presentation is characterized by more gradual onset, and the primary alteration is progressive fluid retention and systemic congestion. New-onset HF is seen much less frequently (less than one-third of HF admissions) than decompensation of chronic HF but may present with the same phenotype. Usual symptoms: ●Progressive dyspnea is the most common complaint of patients presenting with ADHF. ●Symptoms of abdominal and peripheral congestion – Patients may report ankle swelling
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
id retention and systemic congestion. New-onset HF is seen much less frequently (less than one-third of HF admissions) than decompensation of chronic HF but may present with the same phenotype. <span>Usual symptoms: ●Progressive dyspnea is the most common complaint of patients presenting with ADHF. ●Symptoms of abdominal and peripheral congestion – Patients may report ankle swelling and epigastric tenderness or a sensation of abdominal fullness. Abdominal tenderness is often due to hepatic congestion and distention of the hepatic capsule. With severe hepatic congestion, the patient may also complain of nausea and anorexia. ●Other symptoms include nocturia and neurologic symptoms such as confusion, headaches, insomnia, anxiety, disorientation, and impaired memory. Physical signs: ●Vary according to the severity of fluid overload HF. ●Signs of congestion – An elevated jugular venous pressure, positive hepatojugular reflux test, and a tender, enlar
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
erity of fluid overload HF. ●Signs of congestion – An elevated jugular venous pressure, positive hepatojugular reflux test, and a tender, enlarged liver are frequent findings in these patients. <span>Diminished air entry at the lung bases is usually caused by a pleural effusion, which is often more frequent in the right pleural cavity than in the left. Rales (crackles) and wheezing may or may not accompany signs of pleural effusion. An absence of rales does not imply lack of pulmonary venous pressure elevation. Leg edema is frequently
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
e frequent findings in these patients. Diminished air entry at the lung bases is usually caused by a pleural effusion, which is often more frequent in the right pleural cavity than in the left. <span>Rales (crackles) and wheezing may or may not accompany signs of pleural effusion. An absence of rales does not imply lack of pulmonary venous pressure elevation. Leg edema is frequently evident in both legs, particularly in the pretibial region and ankles in ambulatory patients. Sacral and upper thigh edema can be detected in patients who are be
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
leural cavity than in the left. Rales (crackles) and wheezing may or may not accompany signs of pleural effusion. An absence of rales does not imply lack of pulmonary venous pressure elevation. <span>Leg edema is frequently evident in both legs, particularly in the pretibial region and ankles in ambulatory patients. Sacral and upper thigh edema can be detected in patients who are bedridden. ●Cardiac examination – This may be entirely normal in patients with HF secondary to diastolic dysfunction, whereas many patients with advanced systolic dysfunction exhibit a third heart
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
eg edema is frequently evident in both legs, particularly in the pretibial region and ankles in ambulatory patients. Sacral and upper thigh edema can be detected in patients who are bedridden. ●<span>Cardiac examination – This may be entirely normal in patients with HF secondary to diastolic dysfunction, whereas many patients with advanced systolic dysfunction exhibit a third heart sound and a laterally displaced apex beat. A murmur of mitral regurgitation is often audible when the left ventricle (LV) is markedly enlarged, or a tricuspid regurgitation murmur is present when the right ventricle is volume or pressure overloaded. ●Chest radiograph in this setting may show cardiomegaly. Some patients have evidence of pleural effusion and redistribution of blood flow from bases to the upper lobes. There may or may
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
atients have evidence of pleural effusion and redistribution of blood flow from bases to the upper lobes. There may or may not be evidence of interstitial edema. (See 'Chest radiograph' below.) <span>ADHF with severe pulmonary edema — Pulmonary edema has been observed in 15 percent or more of patients admitted with ADHF [13], but severe pulmonary edema is seen in less than 3 percent of these patients [1]. This phenotype is characterized by the rapid onset of symptoms or signs of HF, frequently presenting with a systolic blood pressure >180 mmHg [17]. Patients with this condition frequently have a history of poorly controlled hypertension [18]. There is usually predominant pulmonary rather than systemic congestion, as is manifest by minimal weight gain prior to admission. Clinical findings: ●Patients typically experience a sudden and overwhelming sensation of suffocation and air hunger; this is invariably accompanied by extreme anxiety, cough, expectorat
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
equently have a history of poorly controlled hypertension [18]. There is usually predominant pulmonary rather than systemic congestion, as is manifest by minimal weight gain prior to admission. <span>Clinical findings: ●Patients typically experience a sudden and overwhelming sensation of suffocation and air hunger; this is invariably accompanied by extreme anxiety, cough, expectoration of a pink frothy liquid, and a sensation of drowning. ●The patient sits bolt upright, is unable to speak in full sentences, and may thrash about. The respiratory rate is increased, the alae nasi are dilated, and there is inspiratory retraction of the intercostal spaces and supraclavicular fossae. ●Respiration is often noisy, and there may be audible inspiratory and expiratory gurgling sounds. An ominous sign is obtundation, which may be a sign of severe hypoxemia. Sweating is profuse, and the skin tends to be cool, ashen, and cyanotic, reflecting increased sympathetic outflow. ●The pulse rate is most often elevated secondary to an increased adrenergic drive. When the blood pressure is found to be markedly elevated, it is more likely to be the cause of, or an important contributing factor to, pulmonary edema rather than the consequence of the condition. ●The oxygen saturation is usually less than 90 percent of room air before treatment. Auscultation of the lungs usually reveals coarse airway sounds bilaterally with rhonchi, wheezes, and moist fine crepitant rales that are detected first at the lung bases but then extend upward to the apices as the lung edema worsens. ●Cardiac auscultation may be difficult in the acute situation, but third and fourth heart sounds may be present. When valvular abnormalities and/or mechanical complications after MI result in ADHF, the murmurs of mitral and aortic regurgitation and ischemic ventricular septal defect are often audible, but detection requires a careful and skillful auscultator. (See "Auscultation of cardiac murmurs in adults".) ●The chest radiograph may show cardiomegaly, upper zone redistribution of blood flow, interstitial edema (with ill-defined vessels, peribronchial cuffing, and interlobular septal thicke
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
and aortic regurgitation and ischemic ventricular septal defect are often audible, but detection requires a careful and skillful auscultator. (See "Auscultation of cardiac murmurs in adults".) ●<span>The chest radiograph may show cardiomegaly, upper zone redistribution of blood flow, interstitial edema (with ill-defined vessels, peribronchial cuffing, and interlobular septal thickening), and alveolar edema (with perihilar and lower-lobe airspace filling, with the periphery generally spared in the mid and upper lung zones) [19]. (See 'Chest radiograph' below.) Cardiogenic shock — In one study of patients who presented with acutely decompensated HF, at least one sign of cardiogenic shock (eg, blood pressure <
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
eptal thickening), and alveolar edema (with perihilar and lower-lobe airspace filling, with the periphery generally spared in the mid and upper lung zones) [19]. (See 'Chest radiograph' below.) <span>Cardiogenic shock — In one study of patients who presented with acutely decompensated HF, at least one sign of cardiogenic shock (eg, blood pressure <90 mmHg, cutaneous pallor, mental confusion) was present in 3.6 percent of patients [20]. ●Low-output HF is characterized by symptoms and signs that are related to decreased end-organ perfusion. A typical patient with this clinical syndrome has severely impaired LV function
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
presented with acutely decompensated HF, at least one sign of cardiogenic shock (eg, blood pressure <90 mmHg, cutaneous pallor, mental confusion) was present in 3.6 percent of patients [20]. <span>●Low-output HF is characterized by symptoms and signs that are related to decreased end-organ perfusion. A typical patient with this clinical syndrome has severely impaired LV function and usually presents with symptoms of fatigue, altered mental status, or signs of organ hypoperfusion such as prerenal azotemia or abnormal hepatic enzymes. ●The patient may present with tachypnea at rest, tachycardia, and a cold and cyanotic periphery with poor capillary refill. The degree of peripheral hypoperfusion may be so advanced that the skin over the lower extremities is mottled, cool, or diaphoretic. ●A diminished pulse pressure, consistent with a reduced stroke volume, is often found in patients with this syndrome. Occasionally, the clinician may detect pulsus alternans: when a strong or normal pulse alternates with a weak pulse during normal sinus rhythm. This physical finding is rare but, when present, is a sign of severe LV dysfunction. (See "Examination of the arterial pulse" and "Examination of the arterial pulse", section on 'Pulsus alternans'.) ●A subset of patients with decompensated end-stage HF present with occult shock and may be difficult to distinguish from patients with mildly decompensated chronic HF and stable HF [21]. The only parameter differentiating occult shock patients from nonshock patients is a significantly elevated lactic acid level. Therefore, we suggest checking a lactic acid level in patients who present with marked weakness and/or uncertain peripheral perfusion. (See 'Laboratory data' below.) ●It is imperative to rapidly identify the cardiac causes of shock. After an acute coronary syndrome has been excluded, echocardiography should be done as soon as possible to exclude cardiac tamponade and further characterize left and right ventricular function and the integrity of the left-sided valves. High-output heart failure — This phenotype is an uncommon cause of ADHF and generally presents with warm extremities, pulmonary congestion, tachycardia, and a wide pulse pressure. Under
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
cluded, echocardiography should be done as soon as possible to exclude cardiac tamponade and further characterize left and right ventricular function and the integrity of the left-sided valves. <span>High-output heart failure — This phenotype is an uncommon cause of ADHF and generally presents with warm extremities, pulmonary congestion, tachycardia, and a wide pulse pressure. Underlying conditions include anemia, obesity, thyrotoxicosis, advanced liver failure, and skeletal conditions such as Paget disease. (See "Causes and pathophysiology of high-output heart failure".) Right-sided heart failure — This syndrome of predominantly right-sided HF occurs commonly in patients with severe isolat
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
lying conditions include anemia, obesity, thyrotoxicosis, advanced liver failure, and skeletal conditions such as Paget disease. (See "Causes and pathophysiology of high-output heart failure".) <span>Right-sided heart failure — This syndrome of predominantly right-sided HF occurs commonly in patients with severe isolated tricuspid regurgitation, right ventricular dysfunction, and chronic lung disease, such as those with chronic obstructive lung disease, interstitial lung disease, or long-standing pulmonary hypertension. These patients are often oxygen dependent and present with signs and symptoms of right-sided volume overload. Pulmonary embolism as an acute cause of dyspnea and right HF should be excluded. (See 'Differential diagnosis' below.) DIAGNOSTIC EVALUATION — Initial assessment of ADHF should include a brief, focused history and a physical examination to evaluate signs and symptom
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
the 2010 Heart Failure Society of America [22], the 2013 American College of Cardiology Foundation/American Heart Association [23], and the 2021 European Society of Cardiology guidelines [12]. <span>Initial evaluation for cardiopulmonary instability — The goal of the initial evaluation of patients with ADHF is to determine the patient’s cardiopulmonary status, including the severity of dyspnea, hemodynamic status (evidence of hypoperfusion including hypotension), and heart rate and rhythm. ADHF is a heterogeneous condition, and successful management often relies on identifying the cause of decompensation. The search for specific causes is an essential first step in the ev
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
vidence of hypoperfusion including hypotension), and heart rate and rhythm. ADHF is a heterogeneous condition, and successful management often relies on identifying the cause of decompensation. <span>The search for specific causes is an essential first step in the evaluation of these patients. These include acute coronary syndrome (ACS), hypertensive emergency, rapid arrhythmias or severe bradycardia/conduction disturbance, acute mechanical causes such as acute valve regurgitation or acute pulmonary embolism, infection, including myocarditis, and tamponade. The acronym CHAMPIT (ACS, Hypertension, Arrhythmia, Mechanical causes, Pulmonary embolus, Infection, and Tamponade) was suggested as a useful reminder of the etiologic considerations by
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
arrhythmias or severe bradycardia/conduction disturbance, acute mechanical causes such as acute valve regurgitation or acute pulmonary embolism, infection, including myocarditis, and tamponade. <span>The acronym CHAMPIT (ACS, Hypertension, Arrhythmia, Mechanical causes, Pulmonary embolus, Infection, and Tamponade) was suggested as a useful reminder of the etiologic considerations by the European Society of Cardiology [12]. Symptoms of ACS (eg, chest pain) are assessed and an electrocardiogram (ECG) is obtained and assessed for evidence of ischemia. (See "Initial evaluation and management of suspected acut
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
ained and assessed for evidence of ischemia. (See "Initial evaluation and management of suspected acute coronary syndrome (myocardial infarction, unstable angina) in the emergency department".) <span>Patients with respiratory failure and/or shock — Patients with respiratory distress and/or hypotension require immediate treatment, as discussed separately, followed by an expedited diagnostic evaluation (table 2). (See "Treatment of acute decompensated heart failure: Specific therapies", section on 'Supplemental oxygen and assisted ventilation' and "Treatment of acute decompensated heart failure:
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
therapies", section on 'Supplemental oxygen and assisted ventilation' and "Treatment of acute decompensated heart failure: Specific therapies", section on 'Management of hypotensive patients'.) <span>Patients with acute coronary syndrome — Patients with ADHF with suspected ACS should be promptly identified by ECG and cardiac troponin testing and referred for consideration of cardiac catheterization with coronary angiography and hemodynamic evaluation as appropriate for the condition and prognosis of the patient. The evaluation and management of patients with symptoms and signs of ACS are discussed separately (table 3). (See "Initial evaluation and management of suspected acute coronary syndrome (myocardial infarction, unstable angina) in the emergency department" and "Treatment of acute decompensated
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
atment of acute decompensated heart failure in acute coronary syndromes".) If myocardial ischemia or MI is suspected, cardiac enzymes should be measured to evaluate potential myocardial injury. <span>Of note, troponin is often mildly elevated in ADHF as a result of myocardial injury, myocyte apoptosis, inflammatory mediator activation, and increased myocardial oxygen demand in the setting of fixed coronary disease. Therefore, troponin elevation in ADHF does not necessarily indicate the presence of an ACS. (See "Troponin testing: Clinical use" and "Use of creatine kinase to detect myocardial injury".) Diagnostic approach — ADHF is diagnosed based upon finding a constellation of clinical s
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
of HF as well as potential contributing factors and comorbidities. (See "Heart failure: Clinical manifestations and diagnosis in adults" and "Pathophysiology of cardiogenic pulmonary edema".) ●<span>The diagnosis of ADHF is based primarily on signs and symptoms and supported by appropriate investigations, such as ECG, chest radiograph, biomarkers (B-type natriuretic peptide [BNP] or N-terminal proBNP [NT-proBNP]), and Doppler echocardiography [12,24]. (See 'How to diagnose ADHF' below.) •The diagnosis of decompensated chronic HF is generally straightforward, especially when a patient presents with fluid retention and exertional dyspn
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
lly when a patient presents with fluid retention and exertional dyspnea. It is essential to rule out alternate causes of the patient's symptoms and signs. (See 'Differential diagnosis' below.) •<span>A BNP or NT-proBNP level is obtained when the diagnosis of HF is uncertain. (See 'Initial tests' below.) •An echocardiogram is generally recommended, particularly if this is a first presentation of HF or if there has been abrupt deterioration in the patient’s c
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
nate causes of the patient's symptoms and signs. (See 'Differential diagnosis' below.) •A BNP or NT-proBNP level is obtained when the diagnosis of HF is uncertain. (See 'Initial tests' below.) •<span>An echocardiogram is generally recommended, particularly if this is a first presentation of HF or if there has been abrupt deterioration in the patient’s condition. (See 'Echocardiography' below.) ●Swan-Ganz catheterization is not generally required but is helpful when the diagnosis is uncertain and for management of patients with persistent sympto
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
ation is not generally required but is helpful when the diagnosis is uncertain and for management of patients with persistent symptoms despite treatment of HF. (See 'Swan-Ganz catheter' below.) <span>How to diagnose ADHF — ADHF is a clinical diagnosis based upon the presence of a constellation of symptoms and signs of HF. While test results (eg, natriuretic peptide level, chest radiograph, echocardiogram) are often supportive, the diagnosis cannot be based on a single symptom or sign [25] or test result [26]. The simplest approach is to categorize patients with suspected ADHF into three categories: High probability — ADHF can be diagnosed with high probability in patients with or without prior history of HF: ●Patients with prior history of HF – When a patient with prior history o
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
often supportive, the diagnosis cannot be based on a single symptom or sign [25] or test result [26]. The simplest approach is to categorize patients with suspected ADHF into three categories: <span>High probability — ADHF can be diagnosed with high probability in patients with or without prior history of HF: ●Patients with prior history of HF – When a patient with prior history of HF presents with exertional dyspnea and evidence of fluid retention (ie, elevated jugular venous pressure [JVP] and/or evidence of pulmonary edema and/or peripheral edema), there is a high probability of ADHF [26]. ●Patients with no prior history of HF – When a patient with no prior history of HF presents with new onset orthopnea, elevated JVP, typical chest radiograph findings of pulmonary edema (see 'Chest radiograph' below), and no fever, there is a high probability of ADHF [26]. Intermediate probability — For patients presenting with symptoms of dyspnea who have no prior history of HF but have known cardiac disease, cardiac risk factors (eg, known coronary arte
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
HF presents with new onset orthopnea, elevated JVP, typical chest radiograph findings of pulmonary edema (see 'Chest radiograph' below), and no fever, there is a high probability of ADHF [26]. <span>Intermediate probability — For patients presenting with symptoms of dyspnea who have no prior history of HF but have known cardiac disease, cardiac risk factors (eg, known coronary artery disease, valve disease, diabetes mellitus, or hypertension), or have ECG abnormalities (atrial fibrillation, evidence of left ventricular hypertrophy, or ischemia), and have uncertain JVP and no evidence of pulmonary edema, there is an intermediate probability of ADHF. In this group of patients, testing of serum natriuretic peptide levels (BNP or NT-proBNP) [26], and in some cases also echocardiography, may be helpful. (See 'Natriuretic peptide levels' below.) Low probability — There is low probability of ADHF in patients who present with dyspnea who lack evidence of cardiac disease (including a norma
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
n this group of patients, testing of serum natriuretic peptide levels (BNP or NT-proBNP) [26], and in some cases also echocardiography, may be helpful. (See 'Natriuretic peptide levels' below.) <span>Low probability — There is low probability of ADHF in patients who present with dyspnea who lack evidence of cardiac disease (including a normal ECG) and who have another explanation for dyspnea such as chronic lung disease or pneumonia. Other causes of dyspnea should be evaluated and treated. If uncertainty regarding a possible diagnosis of ADHF persists, further testing (eg, natriuretic peptide level) may be indicated. Clinical categories — Clinical presentations of ADHF can be categorized according to adequacy of peripheral perfusion ("warm" versus "cold") and the presence of congestion ("dry" or "we
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
monia. Other causes of dyspnea should be evaluated and treated. If uncertainty regarding a possible diagnosis of ADHF persists, further testing (eg, natriuretic peptide level) may be indicated. <span>Clinical categories — Clinical presentations of ADHF can be categorized according to adequacy of peripheral perfusion ("warm" versus "cold") and the presence of congestion ("dry" or "wet") (figure 1) [7,27]. Such categorization predicts prognosis and facilitates attention to specific therapies. ●The most common combination of peripheral perfusion and congestion (more than 70 percent of patients with ADHF) is the "warm and wet" clinical profile [1,2]. This group of patients typ
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
heral perfusion ("warm" versus "cold") and the presence of congestion ("dry" or "wet") (figure 1) [7,27]. Such categorization predicts prognosis and facilitates attention to specific therapies. <span>●The most common combination of peripheral perfusion and congestion (more than 70 percent of patients with ADHF) is the "warm and wet" clinical profile [1,2]. This group of patients typically presents with either normal or markedly elevated systolic blood pressure. •The group with normal blood pressure presents largely with significant volume overload with pulmonary and peripheral congestion (cardiac type). •By contrast, patients with the hypertensive profile manifest with fluid redistribution to the lungs and minimal peripheral fluid accumulation (vascular type). This profile of ADHF is often seen in older adult females with labile hypertension and a preserved left ventricular ejection fraction (LVEF). (See 'ADHF with severe pulmonary edema' above.) ●A minority of patients with ADHF (less than 20 percent) present with a "cold and wet" clinical profile. This includes most patients with
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
e). This profile of ADHF is often seen in older adult females with labile hypertension and a preserved left ventricular ejection fraction (LVEF). (See 'ADHF with severe pulmonary edema' above.) <span>●A minority of patients with ADHF (less than 20 percent) present with a "cold and wet" clinical profile. This includes most patients with cardiogenic shock and low-output syndrome. Patients in this category are at increased risk of death and cardiac transplantation at one year compared with patients with HF with reduced EF with a "wet and warm" profile [7]. (See 'Cardiogenic shock' above.) ●Less than 10 percent of patients with ADHF present with a "warm and dry" or "cold and dry" profile. Initial tests — Initial testing in patients with AD
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
ategory are at increased risk of death and cardiac transplantation at one year compared with patients with HF with reduced EF with a "wet and warm" profile [7]. (See 'Cardiogenic shock' above.) <span>●Less than 10 percent of patients with ADHF present with a "warm and dry" or "cold and dry" profile. Initial tests — Initial testing in patients with ADHF includes a 12-lead ECG, chest radiograph, and laboratory tests. Electrocardiogram — A 12-lead ECG is performed soon after the patie
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
with HF with reduced EF with a "wet and warm" profile [7]. (See 'Cardiogenic shock' above.) ●Less than 10 percent of patients with ADHF present with a "warm and dry" or "cold and dry" profile. <span>Initial tests — Initial testing in patients with ADHF includes a 12-lead ECG, chest radiograph, and laboratory tests. Electrocardiogram — A 12-lead ECG is performed soon after the patient presents with ADHF to assess for evidence of ACS (myocardial ischemia or MI) and arrhythmias (eg, atrial fibrillati
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
resent with a "warm and dry" or "cold and dry" profile. Initial tests — Initial testing in patients with ADHF includes a 12-lead ECG, chest radiograph, and laboratory tests. Electrocardiogram — <span>A 12-lead ECG is performed soon after the patient presents with ADHF to assess for evidence of ACS (myocardial ischemia or MI) and arrhythmias (eg, atrial fibrillation). The ECG may also identify other predisposing or precipitating conditions for HF such as left ventricular hypertrophy or left atrial abnormalities (waveform 1). Additional ECG abnormalities may be seen in a patient during an episode of ADHF. These include nonspecific ST and T wave abnormalities. Transient giant negative T waves, global T wave i
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
thmias (eg, atrial fibrillation). The ECG may also identify other predisposing or precipitating conditions for HF such as left ventricular hypertrophy or left atrial abnormalities (waveform 1). <span>Additional ECG abnormalities may be seen in a patient during an episode of ADHF. These include nonspecific ST and T wave abnormalities. Transient giant negative T waves, global T wave inversions, and marked QT interval prolongation have also been reported [28]. These changes may represent subendocardial ischemia (which can be the cause or the result of the pulmonary edema), increase in cardiac sympathetic tone, or metabolic changes. They can also be seen in patients with pulmonary edema due to noncoronary events such as cerebrovascular disease. (See "Neurogenic pulmonary edema".) Chest radiograph — Radiographic findings in ADHF can range from mild pulmonary vascular redistribution to marked cardiomegaly and extensive bilateral
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
e, or metabolic changes. They can also be seen in patients with pulmonary edema due to noncoronary events such as cerebrovascular disease. (See "Neurogenic pulmonary edema".) Chest radiograph — <span>Radiographic findings in ADHF can range from mild pulmonary vascular redistribution to marked cardiomegaly and extensive bilateral interstitial markings (image 1 and image 2 and image 3 and image 4). The presence of bilateral perihilar alveolar edema may give the typical "butterfly" appearance [29]. Unilateral cardiogenic pulmonary edema is infrequent (2 percent of cardiogenic pulmonary edema cases in one study) and is chiefly caused by eccentric mitral regurgitation [30]. Pleural
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
and extensive bilateral interstitial markings (image 1 and image 2 and image 3 and image 4). The presence of bilateral perihilar alveolar edema may give the typical "butterfly" appearance [29]. <span>Unilateral cardiogenic pulmonary edema is infrequent (2 percent of cardiogenic pulmonary edema cases in one study) and is chiefly caused by eccentric mitral regurgitation [30]. Pleural effusions are often absent in patients with de novo ADHF but are frequently present in patients with acute decompensation of chronic HF. Up to 20 percent of patients with ADHF m
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
appearance [29]. Unilateral cardiogenic pulmonary edema is infrequent (2 percent of cardiogenic pulmonary edema cases in one study) and is chiefly caused by eccentric mitral regurgitation [30]. <span>Pleural effusions are often absent in patients with de novo ADHF but are frequently present in patients with acute decompensation of chronic HF. Up to 20 percent of patients with ADHF may have normal chest radiographs [31]. Lung ultrasound — In experienced centers, LUS is an adjunctive diagnostic modality that may be helpful in
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
y caused by eccentric mitral regurgitation [30]. Pleural effusions are often absent in patients with de novo ADHF but are frequently present in patients with acute decompensation of chronic HF. <span>Up to 20 percent of patients with ADHF may have normal chest radiographs [31]. Lung ultrasound — In experienced centers, LUS is an adjunctive diagnostic modality that may be helpful in the evaluation of patients with dyspnea with suspected ADHF [32,33]; it should
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
uld not replace standard clinical assessment (including chest radiograph and selective natriuretic peptide level testing). (See 'Chest radiograph' above and 'Natriuretic peptide levels' below.) <span>The presence of multiple B-lines (generally three or more) per intercostal space on point-of-care ultrasound (LUS) is a sign of lung interstitial syndrome; causes of multiple diffuse bilateral B-lines include pulmonary edema as well as interstitial pneumonia or pneumonitis or diffuse parenchymal lung disease (pulmonary fibrosis) [34]. B-lines are laser-like (also described as comet-like), vertical, hyperechoic artifacts that arise from the pleural line, extend to the bottom of the screen without fading, and move synchronously with lung sliding, as defined by the 2012 International evidence-based recommendations for point-of-care lung ultrasound [34]. (See "Indications for bedside ultrasonography in the critically ill adult patient", section on 'Thoracic ultrasonography'.) Limitations of this modality include technique-dependence and
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
ung disease (pulmonary fibrosis) include pleural line abnormalities (irregular, fragmented), subpleural abnormalities (small echo-poor areas), and a nonhomogeneous distribution of B-lines [34]. <span>Repeated examination may also be helpful since B-lines caused by pulmonary edema vary with volume changes and position (sitting versus supine) [32]. Sonographic findings indicative of acute respiratory distress syndrome include anterior subpleural consolidation, absence or reduction of lung sliding, spared areas of normal parenchyma
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
data are obtained when feasible but are generally not needed to make the diagnosis or guide initial therapy; treatment should NOT be delayed while waiting for the results of laboratory tests. ●<span>Pulse oximetry is often used for initial identification of hypoxia. Arterial blood gas analysis is recommended in all patients with hypoxia and/or severe respiratory distress to assess ventilatory and acid-base status [37]. ●Routine chemistries including serum electrolytes, bicarbonate, blood urea nitrogen (BUN), and serum creatinine are helpful in guiding electrolyte (eg, potassium and magnesium) repletio
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
onate, blood urea nitrogen (BUN), and serum creatinine are helpful in guiding electrolyte (eg, potassium and magnesium) repletion during diuresis and in assessing and monitoring renal function. <span>A decline in renal function is commonly found in patients with advanced HF (cardiorenal syndrome). This may be due in part to a low-output state and elevated central venous pressures. Increased BUN and serum creatinine may also reflect underlying renal disease and, in some cases, may reflect bilateral renal artery stenosis. ●We suggest checking a lactic acid level in patients in shock as well as in those with marked weakness and/or uncertain peripheral perfusion. (See 'Cardiogenic shock' above and "Approac
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
utput state and elevated central venous pressures. Increased BUN and serum creatinine may also reflect underlying renal disease and, in some cases, may reflect bilateral renal artery stenosis. ●<span>We suggest checking a lactic acid level in patients in shock as well as in those with marked weakness and/or uncertain peripheral perfusion. (See 'Cardiogenic shock' above and "Approach to the adult with metabolic acidosis".) ●Serum troponin (T or I) levels are obtained in any patient with possible ACS. For patients with cri
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
level in patients in shock as well as in those with marked weakness and/or uncertain peripheral perfusion. (See 'Cardiogenic shock' above and "Approach to the adult with metabolic acidosis".) ●<span>Serum troponin (T or I) levels are obtained in any patient with possible ACS. For patients with criteria for ST elevation MI, reperfusion therapy (percutaneous coronary intervention or thrombolysis) should not be delayed to wait for the results of troponin measur
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
gement of suspected acute coronary syndrome (myocardial infarction, unstable angina) in the emergency department" and "Overview of the acute management of ST-elevation myocardial infarction".) ●<span>A complete blood count may help identify the presence of infection or anemia that may have precipitated the event. (See "Evaluation and management of anemia and iron deficiency in adults with heart failure".) Natriuretic peptide levels — If the diagnosis of HF is uncertain in a patient with dyspnea
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
iuretic peptide levels — If the diagnosis of HF is uncertain in a patient with dyspnea and other signs and symptoms suggestive of ADHF, plasma BNP or NT-proBNP concentration should be measured. <span>Decision analysis suggests that BNP or NT-proBNP testing is generally most useful in patients who have an intermediate probability of HF [38]. The natriuretic peptide concentration should not be interpreted in isolation but in the context of all available clinical data bearing on the diagnosis of ADHF. (See 'How to diagnose ADHF' above.) Most dyspneic patients with HF have plasma BNP values above 400 pg/mL. For patients <50, 50 to 75, and >75 years of age, the optimal plasma NT-
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
natriuretic peptide concentration should not be interpreted in isolation but in the context of all available clinical data bearing on the diagnosis of ADHF. (See 'How to diagnose ADHF' above.) <span>Most dyspneic patients with HF have plasma BNP values above 400 pg/mL. For patients <50, 50 to 75, and >75 years of age, the optimal plasma NT-proBNP cutoffs for diagnosing HF are 450, 900, and 1800 pg/mL, respectively. (See "Natriuretic peptide measurement in heart failure".) There is considerable overlap in BNP and NT-proBNP levels in patients with and without HF, which makes the test less robust in
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
, 50 to 75, and >75 years of age, the optimal plasma NT-proBNP cutoffs for diagnosing HF are 450, 900, and 1800 pg/mL, respectively. (See "Natriuretic peptide measurement in heart failure".) <span>There is considerable overlap in BNP and NT-proBNP levels in patients with and without HF, which makes the test less robust in an individual patient with intermediate levels of BNP (approximately 200 to 400 pg/mL). Since many conditions increase natriuretic peptide levels, low values of BNP (<100 pg/mL) or NT-proBNP (<300 pg/mL) are most useful because the diagnosis of ADHF is very unlikely as an explanation for dyspnea [39]. However, unexpectedly low natriuretic peptide levels are occasionally found in some patients with end-stage HF, acute pulmonary edema, and right-sided HF [12]. Results of BNP or NT-proB
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
ase natriuretic peptide levels, low values of BNP (<100 pg/mL) or NT-proBNP (<300 pg/mL) are most useful because the diagnosis of ADHF is very unlikely as an explanation for dyspnea [39]. <span>However, unexpectedly low natriuretic peptide levels are occasionally found in some patients with end-stage HF, acute pulmonary edema, and right-sided HF [12]. Results of BNP or NT-proBNP testing must be interpreted with caution, and such testing must support rather than override careful clinical judgment. (See "Natriuretic peptide measurement
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
an explanation for dyspnea [39]. However, unexpectedly low natriuretic peptide levels are occasionally found in some patients with end-stage HF, acute pulmonary edema, and right-sided HF [12]. <span>Results of BNP or NT-proBNP testing must be interpreted with caution, and such testing must support rather than override careful clinical judgment. (See "Natriuretic peptide measurement in heart failure" and "Natriuretic peptide measurement in heart failure", section on 'BNP and the diagnosis of HF in the patient with dyspnea' and
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
t failure", section on 'BNP and the diagnosis of HF in the patient with dyspnea' and "Natriuretic peptide measurement in heart failure", section on 'Acute decompensated HF'.) Echocardiography — <span>Echocardiography is recommended for patients with new HF and for patients with prior history of HF with suspected change in cardiac function. The urgency of echocardiography varies with the acuity of presentation. This imaging modality should be utilized early on during the evaluation of patients with cardiogenic shock or low-output syndrome. This imaging modality is also critical in the evaluation of patients with known or suspected valvular heart disease. In patients with ST elevation MI and pulmonary congestion, echocardi
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
tion. When reduced LVEF (<40 percent) is found, the cause of HF may be ascribed to systolic dysfunction (with or without other causes such as diastolic dysfunction or valvular disease) [37]. <span>When preserved LV systolic function is found, the cause of HF may be diastolic dysfunction, transient systolic dysfunction, other causes of HF with preserved EF including valvular heart disease (table 4), or diagnostic error (no HF with symptoms/signs due to another cause). Additional tests Swan-Ganz catheter — Routine use of invasive hemodynamic monitoring in patients with ADHF is NOT recommended [22,40]. Available evidence on flow-directed pulmonary arte
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
le Access Help & Training Demos Wolters Kluwer Health Emmi® Facts & Comparisons® Lexicomp® Medi-Span® Loading Please wait 4 of 11 Export to Powerpoint Print Share Bookmark Rate Feedback <span>Differential diagnosis of heart failure with preserved ejection fraction Heart failure with preserved ejection fraction (HFpEF) HFpEF (contributing factors include hypertension, aging, coronary heart disease, diabetes mellitus, sleep-disordered breathing, chronic kidney disease, and obesity) Cardiomyopathies with preserved ejection fraction Restrictive cardiomyopathy Familial causes include sarcomeric gene mutations, familial amyloidosis (transthyretin [TTR] or apolipoprotein mutation), unknown gene mutation, familial causes of iron overload (hereditary hemochromatosis, hereditary anemias), Fabry disease, glycogen storage disease, desminopathy, and pseudoxanthoma elasticum Nonfamilial causes include amyloid (immunoglobulin light chain [AL] or wild-type transthyretin [ATTR]), systemic sclerosis, endomyocardial fibrosis (idiopathic, caused by hypereosinophilic syndrome, or reaction to a drug), carcinoid heart disease, metastatic cancer, radiation, nonfamilial iron overload (eg, acquired iron-loading anemia, high-dietary intake), and drug toxicity (anthracycline) Hypertrophic cardiomyopathy Familial causes in addition to sarcomere gene mutations include unknown mutations, glycogen storage disease, lysosomal storage disease (including Fabry disease), syndromic hypertrophic cardiomyopathy (eg, Noonan syndrome, LEOPARD syndrome, Friedreich ataxia), and familial amyloidosis (TTR or apolipoprotein mutation) Nonfamilial causes include nonfamilial amyloidosis (AL or wild-type ATTR) Noncompaction cardiomyopathy Valvular heart disease Valvular stenosis Valvular regurgitation Right heart failure Pulmonary hypertension Right ventricular infarction Arrhythmogenic right ventricular cardiomyopathy Pericardial disease Cardiac tamponade Constrictive pericarditis Effusive-constrictive pericardial disease Obstructive lesion in heart or great vessel Atrial myxoma Pulmonary vein stenosis High-output heart failure Transient left ventricular systolic dysfunction Adapted from: Oh JK, Hatle L, Tajik AJ, Little WC. Diastolic heart failure can be diagnosed by comprehensive two-dimensional and Doppler echocardiography. J Am Coll Cardiol 2006; 47:500
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
one or more of the following conditions: ●Renal function is worsening with therapy ●Parenteral vasoactive agents are required ●Advanced device therapy or cardiac transplantation may be required <span>A pulmonary capillary wedge pressure or its equivalent, pulmonary artery occlusion pressure, of ≥18 mmHg favors cardiogenic pulmonary edema. (See "Pulmonary artery catheterization: Indications, contraindications, and complications in adults" and "Pulmonary artery catheterization: Interpretation of hemodynamic values and wave
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
onary artery catheterization: Indications, contraindications, and complications in adults" and "Pulmonary artery catheterization: Interpretation of hemodynamic values and waveforms in adults".) <span>However, it is important to appreciate that pulmonary artery catheterization measurements can be misleading in certain settings. Most importantly, intermittent myocardial ischemia can cause severe but transient reduction in LV compliance, accompanied by an elevation in the LV filling pressure. Because of the change in ventricular compliance, this elevation in pressure may or may not be accompanied by an elevation in the LV volume. Furthermore, if the pulmonary capillary wedge
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
resolved (and if LV function has improved), a relatively normal value may be obtained, leading to the erroneous conclusion that the respiratory distress was caused by noncardiogenic mechanisms. <span>On the other hand, an elevated wedge pressure does not exclude the possibility of noncardiogenic pulmonary edema. It is estimated that as many as 20 percent of patients with pulmonary edema due to acute respiratory distress syndrome (ARDS) have concomitant LV dysfunction. The contribution of ARDS to the pulmonary edema requires monitoring the wedge pressure response to treatment. Noncardiogenic factors are probable if the pulmonary infiltrates and hypoxemia do not improve appreciably within 24 to 48 hours after normalization of the wedge pressure. (See "Noncardiogenic pulmonary edema".) In patients with adequate acoustic windows, echocardiography may provide a noninvasive means of estimating filling pressures. (See "Tissue Dopple
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
resents with the sudden onset of respiratory distress that may or may not be associated with chest discomfort or a previous history of heart disease, other medical conditions must be excluded: ●<span>Pulmonary embolism – The sudden onset of dyspnea, pleuritic chest pain, and cough may be caused by a pulmonary embolism. Establishing the diagnosis may depend upon the characteristics of the ECG and the differences in appearance of typical chest radiograph findings in the two conditions. (See "Clinical presentation, evaluation, and diagnosis of the nonpregnant adult with suspected acute pulmonary embolism".) In addition to being part of the differential diagnosis, venou
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
appearance of typical chest radiograph findings in the two conditions. (See "Clinical presentation, evaluation, and diagnosis of the nonpregnant adult with suspected acute pulmonary embolism".) <span>In addition to being part of the differential diagnosis, venous thromboembolism is more common in patients with HF and, in patients with ADHF, is associated with a worse prognosis [42]. (See "Antithrombotic therapy in patients with heart failure".) ●Pneumonia – Pneumonia can present with acute shortness of breath, hypoxemia, and an inconclusive pulmonary examination. C
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
venous thromboembolism is more common in patients with HF and, in patients with ADHF, is associated with a worse prognosis [42]. (See "Antithrombotic therapy in patients with heart failure".) ●<span>Pneumonia – Pneumonia can present with acute shortness of breath, hypoxemia, and an inconclusive pulmonary examination. Chest radiograph findings may differ, but some cases of bibasilar pneumonia may be similar to HF, although evidence of upper zone redistribution is not present with pneumonia. Fever and leukocytosis may suggest an infectious process. (See "Clinical evaluation and diagnostic testing for community-acquired pneumonia in adults".) ●Asthma – Reactive airways disease can cause acute shortness of breath, cough, and fatigue
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
ribution is not present with pneumonia. Fever and leukocytosis may suggest an infectious process. (See "Clinical evaluation and diagnostic testing for community-acquired pneumonia in adults".) ●<span>Asthma – Reactive airways disease can cause acute shortness of breath, cough, and fatigue. In addition, patients with ADHF may present with wheezing that can simulate asthma. The chest radiograph can be helpful in differentiating these conditions. (See "Asthma in adolescents and adults: Evaluation and diagnosis".) ●Noncardiogenic pulmonary edema (NCPE) – NCPE is invariably associated with an underlying disease, which may or may n
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
may present with wheezing that can simulate asthma. The chest radiograph can be helpful in differentiating these conditions. (See "Asthma in adolescents and adults: Evaluation and diagnosis".) ●<span>Noncardiogenic pulmonary edema (NCPE) – NCPE is invariably associated with an underlying disease, which may or may not be readily apparent. The diagnosis of NCPE often depends on pretest probabilities: acute respiratory distress in a patient with documented sepsis (ie, peritonitis) or pancreatitis should raise the strong possibility that the respiratory failure is due to NCPE. In contrast to cardiogenic pulmonary edema (CPE), NCPE is uncommonly associated with a well-defined acute cardiac event (ie, MI). Subtle physical signs may also aid in differentiating NCPE from CPE. NCPE is usually a hyperdynamic illness, clinically apparent as a warm, vasodilated periphery, whereas CPE is frequen
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
strong possibility that the respiratory failure is due to NCPE. In contrast to cardiogenic pulmonary edema (CPE), NCPE is uncommonly associated with a well-defined acute cardiac event (ie, MI). <span>Subtle physical signs may also aid in differentiating NCPE from CPE. NCPE is usually a hyperdynamic illness, clinically apparent as a warm, vasodilated periphery, whereas CPE is frequently associated with a cold and sweaty periphery. Tachycardia is frequently present with NCPE or CPE. The findings of a third heart sound or murmurs of aortic and mitral regurgitation and aortic stenosis suggest a cardiogenic cause of pulmonary edema. ST segment changes on ECG consistent with MI or myocardial ischemia would suggest an acute cardiac event as the cause of the pulmonary edema. Also, ECG evidence of left ventricular stra
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
her abnormalities of the QRS complex might indicate an underlying cardiac pathology. By contrast, the ECG is usually normal in patients with NCPE, unless there are major metabolic disturbances. <span>In NCPE and CPE, arterial hypoxemia is due to changes in the ventilation-perfusion ratio and in the extent of intrapulmonary shunting. Patients with NCPE usually have a more pronounced defect in oxygenation than is seen in patients with CPE, largely due to the greater shunt fractions found in these patients. Higher concentrations of inspired oxygen concentrations (FiO2) and larger positive end-expiratory pressures are often required to achieve acceptable oxygenation in NCPE compared with CPE (table 5). (See "Noncardiogenic pulmonary edema".) FOLLOW-UP AND DISPOSITION Monitoring — Monitoring of a patient with ADHF should be initiated as soon as possible after admission to the emergency department. The type and level of monit
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
ergency department. The type and level of monitoring required for any individual patient vary widely depending on the severity of the cardiac decompensation and the response to initial therapy. <span>Generally, the following parameters should be measured in all critically ill patients: mental status, blood pressure, temperature, respiratory rate, heart rate, and urine output. Some laboratory tests should be monitored by repeated testing (eg, electrolytes, creatinine, glucose). Liver function tests and lactate levels should be measured when there is evidence
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
ental status, blood pressure, temperature, respiratory rate, heart rate, and urine output. Some laboratory tests should be monitored by repeated testing (eg, electrolytes, creatinine, glucose). <span>Liver function tests and lactate levels should be measured when there is evidence of hypoperfusion. Arterial blood gas analysis is generally not routinely required but is indicated in patients with hypoxia and/or respiratory failure. After admission to the intensive care unit (ICU) or a step down unit, patients with ADHF should be carefully monitored to ensure that the treatment goals are met and continued progress
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
UpToDate
nt — Patients with severe respiratory failure and patients in shock or preshock should be admitted to the ICU. In North America, 10 to 12 percent of patients with ADHF are managed in ICUs [51]. <span>Although no validated algorithms exist at this time to guide the clinician for triaging patients with decompensated chronic HF to regular floor beds or to the ICU, we agree that presence of one or more of the following conditions is generally a criterion for admission to an ICU as described in the 2021 European Society of Cardiology HF guidelines and by other experts [12,52]: ●Patient is intubated or likely to require respiratory support/intubation. This includes patients with either of the following characteristics: •Arterial oxygen saturation (SpO2 ≤90 percent) despite supplemental oxygen. •Patient is using accessory muscles and respiratory rate is ≥25 breaths/minute. ●Signs and symptoms of hypoperfusion and/or systolic blood pressure <90 mmHg. ●Heart rate <40 or >130 beats/minute. SOCIETY GUIDELINE LINKS — Links to society and government-sponsored guidelines from selected countries and regions around the world are provided separately. (See "Society guideline link