Edited, memorised or added to reading queue
on 05-Feb-2017 (Sun)
Do you want BuboFlash to help you learning these things? Click here to log in or create user.
Flashcard 1425614966028
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itThis reading is organized as follows. Section 2 explains how economists classify markets. Section 3 covers the basic principles and concepts of demand and supply analysis of markets. Section 4 introduces measures of sensitivity of demand to changes in prices and income. <span><body><html>
Original toplevel document
1. INTRODUCTIONs to converge to an equilibrium price? What are the conditions that would make that equilibrium stable or unstable in response to external shocks? How do different types of auctions affect price discovery? <span>This reading is organized as follows. Section 2 explains how economists classify markets. Section 3 covers the basic principles and concepts of demand and supply analysis of markets. Section 4 introduces measures of sensitivity of demand to changes in prices and income. A summary and practice problems conclude the reading. <span><body><html>
Flashcard 1429338983692
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itA practical, normative study is one that seeks to regulate, to bring into conformity with a norm or standard—for example, ethics. The norm of ethics is the good, and its purpose is to bring human conduct into
Original toplevel document (pdf)
cannot see any pdfsFlashcard 1432952638732
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itA genus is a wider class made up of two or more different species that have in common the same generic essence or nature.
Original toplevel document (pdf)
cannot see any pdfsFlashcard 1432967843084
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itIf a Greek shipping company transports the wine that the United States imports from France, the United States would classify the cost of shipping as an import of services from Greece and the wine would be classified as an import of goods from France.
Original toplevel document
2.1. Basic Terminologyth from India and wine from France. Exports are goods and services that a domestic economy sells to other countries. For example, South Africa exports (sells) diamonds to the Netherlands, and China exports clothing to the European Union. So <span>how are services imported or exported? If a Greek shipping company transports the wine that the United States imports from France, the United States would classify the cost of shipping as an import of services from Greece and the wine would be classified as an import of goods from France. Similarly, when a British company provides insurance coverage to a South African diamond exporter, Britain would classify the cost of the insurance as an export of services to South Afr
Flashcard 1432997989644
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itIn metaphysics, extension signifies both 'stretching out' (Latin: extensio) as well as later 'taking up space', and most recently, spreading one's internal mental cognition into the external world.
Original toplevel document
Extension (metaphysics) - Wikipediaan>Extension (metaphysics) - Wikipedia Extension (metaphysics) From Wikipedia, the free encyclopedia Jump to: navigation, search In metaphysics, extension signifies both 'stretching out' (Latin: extensio) as well as later 'taking up space', and most recently, spreading one's internal mental cognition into the external world. The history of thinking about extension can be traced back at least to Archytas' spear analogy for the infinity of space. How far can one's hand or spear stretch out until it reaches
Flashcard 1438573006092
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itTo represent our consumer’s preferences graphically, not just mathematically, we have the concept of an indifference curve , which represents all the combinations of two goods such that the consumer is entirely indifferent among them.
Original toplevel document
3. UTILITY THEORY: MODELING PREFERENCES AND TASTESweaker measures than cardinal rankings because they do not allow the calculation and ranking of the differences between bundles. 3.3. Indifference Curves: The Graphical Portrayal of the Utility Function <span>It will be convenient for us to represent our consumer’s preferences graphically, not just mathematically. To that end, we introduce the concept of an indifference curve , which represents all the combinations of two goods such that the consumer is entirely indifferent among them. This is how we construct such a curve: Consider bundles that contain only two goods so that we can use a two-dimensional graph to represent them—as in Exhibit 1, where a particular bund
Flashcard 1471451630860
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itg of material from the Earth’s interior (Figure 1–11). Downward-percolating seawater is heated and driven back upward as a submarine geyser, carrying with it a current of chemicals from the hot rocks below. A typical cocktail might include <span>H 2 S, H 2 , C O, Mn 2+ , Fe 2+ , Ni 2+ , CH 2 , NH 4 + , and phosphorus-containing compounds. <span><body><html>
Original toplevel document (pdf)
cannot see any pdfs| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Flashcard 1473235520780
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
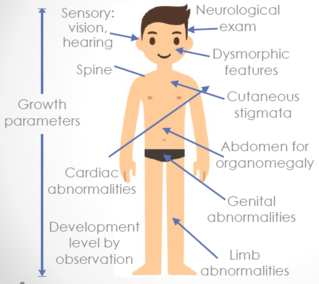
Tricking Kids into the Perfect Exam: Tips for Evaluating the Pediatric Patient
unicate or cooperate with the physical exam. While each physician may vary with style points and favorite tricks, here are a few tips for the pediatric physical exam to improve your interaction and comfort level. <span>One of the fi rst tasks as an emergency physician is to put the patient at ease. Talk to the child as well as the parents. For older children, introduce yourself to them fi rst before the parents and sit down on the bed or chair as to not tower over them. Try to facilitate the relationship and open up communication by noticing something cool about them (i.e. light-up shoes, Dora T-shirt or fun toy). While doing the actual physical exam, try to use the parent’s lap as much as possible as the child is most comfortable there. To distract and calm them, consider tel
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Tricking Kids into the Perfect Exam: Tips for Evaluating the Pediatric Patient
rents and sit down on the bed or chair as to not tower over them. Try to facilitate the relationship and open up communication by noticing something cool about them (i.e. light-up shoes, Dora T-shirt or fun toy). <span>While doing the actual physical exam, try to use the parent’s lap as much as possible as the child is most comfortable there. To distract and calm them, consider telling them a story throughout the exam or try to make the physical exam a game – play with the instruments. Finally, consider having something fun in your pocket such as stickers or a bubble-blowing pen to make the experience more enjoyable. In general, when evaluating any
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Tricking Kids into the Perfect Exam: Tips for Evaluating the Pediatric Patient
arent’s lap as much as possible as the child is most comfortable there. To distract and calm them, consider telling them a story throughout the exam or try to make the physical exam a game – play with the instruments. <span>Finally, consider having something fun in your pocket such as stickers or a bubble-blowing pen to make the experience more enjoyable. In general, when evaluating any child, observation is the best initial diagnostic tool. The degree of alertness and interaction, responsiveness to parents and r
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Tricking Kids into the Perfect Exam: Tips for Evaluating the Pediatric Patient
xam a game – play with the instruments. Finally, consider having something fun in your pocket such as stickers or a bubble-blowing pen to make the experience more enjoyable. In general, when evaluating any child, <span>observation is the best initial diagnostic tool. The degree of alertness and interaction, responsiveness to parents and respiratory status are all valuable measures of illness that may either suggest or eliminate concerns of toxicity. After observation, it is important to begin the exam with auscultation of the heart and lungs as this is usually when the child is calm, quiet and most cooperative.
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Tricking Kids into the Perfect Exam: Tips for Evaluating the Pediatric Patient
t initial diagnostic tool. The degree of alertness and interaction, responsiveness to parents and respiratory status are all valuable measures of illness that may either suggest or eliminate concerns of toxicity. <span>After observation, it is important to begin the exam with auscultation of the heart and lungs as this is usually when the child is calm, quiet and most cooperative. Do not forget that a negative lung auscultation is not suffi cient to rule out signifi cant pulmonary disease; the appearance of the patient (tachypnea, respiratory distress) is much more predictive. Finally, always save the worst for last. The last items to perform in the physical exam should always be those things that are most threatening to the child, includi
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Tricking Kids into the Perfect Exam: Tips for Evaluating the Pediatric Patient
e lung auscultation is not suffi cient to rule out signifi cant pulmonary disease; the appearance of the patient (tachypnea, respiratory distress) is much more predictive. Finally, always save the worst for last. <span>The last items to perform in the physical exam should always be those things that are most threatening to the child, including looking in the ears and mouth. Here are a few cases to illustrate the importance of the physical exam and emphasize other tips for evaluating those age groups that provide the most anxiety an
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Tricking Kids into the Perfect Exam: Tips for Evaluating the Pediatric Patient
3; looking in the ears and mouth. Here are a few cases to illustrate the importance of the physical exam and emphasize other tips for evaluating those age groups that provide the most anxiety and diffi cult exam. <span>Newborn Case 1: A 3-week-old male presented to the emergency department for congestion and cough. Mom stated that the infant was not eating as well, but had normal wet diapers. No fever noted at home or on exam. As mentioned above, it is important to observe the newborn. One of the best tips is to undress and hold the baby. Holding allows the clinician to assess multiple things at once, including level of alertness, respiratory status and tone. This initial assessment gives the clinician a good sense of “sick or not sick.” It is also important to have the baby undressed to do a careful examination, looking for rashes, bruises, hair tourniquets, etc. During the exam, this newborn was observed to have an apneic episode. The patient was admitted for an evaluation that ultimately revealed a diagnosis of pertussis. Infant Case 2: A 5-month-old male presented with fever and fussiness. The patient was seen fi ve days earlier with fever and URI, diagnosed with otitis media and disch
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Tricking Kids into the Perfect Exam: Tips for Evaluating the Pediatric Patient
king for rashes, bruises, hair tourniquets, etc. During the exam, this newborn was observed to have an apneic episode. The patient was admitted for an evaluation that ultimately revealed a diagnosis of pertussis. <span>Infant Case 2: A 5-month-old male presented with fever and fussiness. The patient was seen fi ve days earlier with fever and URI, diagnosed with otitis media and discharged home with amoxicillin. Prior to arrival, the patient had multiple episodes of vomiting and decreased urine output. Initial assessment revealed an illappearing, febrile infant. While observing the infant and beginning the physical exam, it is important to place your hand on the infant’s head and assess the fontanelle. A fontanelle is measured as full, fl at, or depressed. Cup your palm on the back of Rose House, MD EM/Pediatrics Resident Indiana University Indianapolis, IN “In general, when evaluating any child, observation is the best initial diagnostic tool.” 34 EMResident the baby’s head and then move forward. The curve of your palm should touch the fontanelle if it is normal. If the fontanelle doesn’t touch, it is depressed; if it pushes your hand up, it is full. In young infants, a bulging fontanelle may be seen with meningitis, but meningismus is rare before one year of age. Another possible exam fi nding in infants with meningitis is a paradoxical response to consoling maneuvers like cuddling. When a caregiver “cuddles” an infant, the meninges are stretched and irritated making the infant more fussy. By contrast, the same infant will calm when laid fl at. This infant’s fontanelle was full and tense. Throughout the exam, the patient was irritable and diffi cult to console. The infant was appropriately resuscitated and underwent a full septic work-up, revealing pneumococcal meningitis. Toddler Case 3: An 18-month-old male presents with complaint of seizure witnessed at home 20 minutes prior to arrival. Many pediatric patients will present to&#
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Tricking Kids into the Perfect Exam: Tips for Evaluating the Pediatric Patient
elle was full and tense. Throughout the exam, the patient was irritable and diffi cult to console. The infant was appropriately resuscitated and underwent a full septic work-up, revealing pneumococcal meningitis. <span>Toddler Case 3: An 18-month-old male presents with complaint of seizure witnessed at home 20 minutes prior to arrival. Many pediatric patients will present to the emergency department after a seizure. When evaluating this patient, it is crucial to do a good neurological exam. The biggest tip for the pediatric neurological exam is to stop, look and listen. You will learn the most from the child’s spontaneous activity, including mental status, cranial nerves, coordination, and motor status. Assess patients based on developmental milestones for their age group. If age appropriate, make sure to watch them walk. Also, watch the child sit unsupported as truncal instability may be a clue to vertiginous symptoms or cerebellar pathology. Try to carry one thing that could fake for a toy or draw a face on a tongue depressor to help attract the child’s attention. Upon examination of this patient, he had right-sided weakness which resolved within an hour. The patient was diagnosed with Todd’s paralysis and new-onset seizure disorder. Preschooler Case 4: A 3-year-old female presents with abdominal pain and fever over the past day. Patient has some vomiting and diarrhea. Emesis is nonbilious&#
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Tricking Kids into the Perfect Exam: Tips for Evaluating the Pediatric Patient
elp attract the child’s attention. Upon examination of this patient, he had right-sided weakness which resolved within an hour. The patient was diagnosed with Todd’s paralysis and new-onset seizure disorder. <span>Preschooler Case 4: A 3-year-old female presents with abdominal pain and fever over the past day. Patient has some vomiting and diarrhea. Emesis is nonbilious and nonbloody. Diarrhea is watery and yellow. The patient has also had decreased oral intake and urine output. On exam, the patient is febrile and appears uncomfortable. Performing a good abdominal exam is critical for the assessment of this patient, but can often be challenging. Children Figure 1: Additional Tips & Tricks General Always undress. Eyes If trying to get a newborn to open their eyes, holding the infant’s head and dipping it down will cause them to open their eyes. Never try to pry a baby’s eyes open when they are crying as you will not be able to over power them and will just anger them more. Infants should fi x and follow a moving object with both eyes by 3 months of age. Use bright objects or noises to help assess extraocular movements. Ears If having a hard time looking in the ears, hold arms above head. If unable to turn their head, wiggle the otoscope light in front of their eyes and then move it to the opposite side of the ear you want to look in. The child will often track with the light and turn their head so their ear is then right in front of you. Have parent stabilize the head. Use one hand to grab the pinna while holding the otoscope with the thumb and index fi nger and using the little fi nger and heel of the hand to stabilize the otoscope against the side of the face (See Figure 2).2 Mouth/Throat Wetting the tongue depressor makes it taste better. Have the child pant like a dog when doing a throat swab as it helps prevent gagging. Heart If worried about murmurs, gently and briefl y blow in the face of a neonate which slows down their heart rate momentarily so that you can better ausculate for murmurs. Lungs If you want them to take a deep breath, can have them blow out the light on the otoscope or can ask them to pretend to blow out the birthday candles. cannot developmentally pinpoint the location of abdominal pain until they are at least four years old, and perhaps not even then. With symptoms and an exam that are nonspecifi c, abdominal pathology can be very diffi cult to diagnose in this age group. Attempt to calm and distract the patient as much as possible. For infants, make sure to have a pacifi er available during the abdominal exam. Another option for the crying infant is to use sucrose to calm them during auscultation and palpation. Flexing the hips will also facilitate relaxation and a better exam. For patients that are ticklish, you can have the child place their hand on yours and push down as if they are doing the exam. For children with abdominal pain, make sure to always undress the patient and evaluate for rashes to assure that diseases like HenochSchönlein Purpura (HSP) are not missed. Also, referred pain is very common, and pneumonia or strep throat may present with abdominal pain of any location with focal or diffuse pain on exam. Using the above techniques, the patient in the case was found to have signifi cant tenderness without rebound. Upon further evaluation, the patient was found to have acute appendicitis. The above tips and tricks should allow for a smoother encounter with the pediatric patient. If the tactics are not working, do your physical exam in stages. Start quickly with the most essential, then return frequently to perform each additional layer. Always remember that a graceful approach will go a long way with assessing children. <span><body><html>
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Tricking Kids into the Perfect Exam: Tips for Evaluating the Pediatric Patient
sed oral intake and urine output. On exam, the patient is febrile and appears uncomfortable. Performing a good abdominal exam is critical for the assessment of this patient, but can often be challenging. Children <span>Figure 1: Additional Tips & Tricks General Always undress. Eyes If trying to get a newborn to open their eyes, holding the infant’s head and dipping it down will cause them to open their eyes. Never try to pry a baby’s eyes open when they are crying as you will not be able to over power them and will just anger them more. Infants should fi x and follow a moving object with both eyes by 3 months of age. Use bright objects or noises to help assess extraocular movements. Ears If having a hard time looking in the ears, hold arms above head. If unable to turn their head, wiggle the otoscope light in front of their eyes and then move it to the opposite side of the ear you want to look in. The child will often track with the light and turn their head so their ear is then right in front of you. Have parent stabilize the head. Use one hand to grab the pinna while holding the otoscope with the thumb and index fi nger and using the little fi nger and heel of the hand to stabilize the otoscope against the side of the face (See Figure 2).2 Mouth/Throat Wetting the tongue depressor makes it taste better. Have the child pant like a dog when doing a throat swab as it helps prevent gagging. Heart If worried about murmurs, gently and briefl y blow in the face of a neonate which slows down their heart rate momentarily so that you can better ausculate for murmurs. Lungs If you want them to take a deep breath, can have them blow out the light on the otoscope or can ask them to pretend to blow out the birthday candles. cannot developmentally pinpoint the location of abdominal pain until they are at least four years old, and perhaps not even then. With symptoms and an exam that are&
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Highlight doc Day 1
BIOETHICS : Informed Consent (c.f. assent): 1) appropriate info 2) decision-making capacity 3) voluntariness (←the 3 hallmarks of informed consent) Confidentiality Age not a factor Unless teen is Suicidal, homicidal, has thoughts of self-harm/harming others <16yo w/ hx of current/past abuse Disclosu
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Highlight doc Day 1
BIOETHICS : Informed Consent (c.f. assent): 1) appropriate info 2) decision-making capacity 3) voluntariness (←the 3 hallmarks of informed consent) Confidentiality Age not a factor Unless teen is Suicidal, homicidal, has thoughts of self-harm/harming others <16yo w/ hx of current/past abuse Disclosure of abuse & children <16yo in home Capacity & consent Capable if Able to UNDERSTAND info relevant to making decision re: tx Eg I’ll lose my leg if I don’t manage my DM &#
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Highlight doc Day 1
Confidentiality Age not a factor Unless teen is Suicidal, homicidal, has thoughts of self-harm/harming others <16yo w/ hx of current/past abuse Disclosure of abuse & children <16yo in home <span>Capacity & consent Capable if Able to UNDERSTAND info relevant to making decision re: tx Eg I’ll lose my leg if I don’t manage my DM And able to APPRECIATE consequences of a decision Eg of no appreciation: That’s in the future so I don’t care if I’ll lose my leg, I want to live my life now Assume everyone’s capable. Don’t assume incapability b/c Age, Refusal/Disagreement w/ tx, Request for alt tx, Psych/neuro dx, Disability Healthcare decisions for ped pts should be made jointly by health care team, parents, & child/adoles to varying deg Assent = children given info they understand & some appropriate choice in tx Sexual consent (Ontario): 12-13yo ± 2, 14-15yo ± 5, 16yo (no porn, prostitution, autho
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Highlight doc Day 1
/c Age, Refusal/Disagreement w/ tx, Request for alt tx, Psych/neuro dx, Disability Healthcare decisions for ped pts should be made jointly by health care team, parents, & child/adoles to varying deg <span>Assent = children given info they understand & some appropriate choice in tx Sexual consent (Ontario): 12-13yo ± 2, 14-15yo ± 5, 16yo (no porn, prostitution, authority) ETHICAL PRINCIPLES Mother doesn’t want her child to
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Highlight doc Day 1
ity Healthcare decisions for ped pts should be made jointly by health care team, parents, & child/adoles to varying deg Assent = children given info they understand & some appropriate choice in tx <span>Sexual consent (Ontario): 12-13yo ± 2, 14-15yo ± 5, 16yo (no porn, prostitution, authority) ETHICAL PRINCIPLES Mother doesn’t want her child to be vaccinated. Which ethical principle would you apply to give the vaccine to the child who doesn’t
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Highlight doc Day 1
tand relevant info (risks, benefits) 2) appreciate consequences Disagree: 1) best interests of the child (non-maleficence, beneficence), 2) justice Agree: 1) best interests of the child (non-maleficence, beneficence), 2) family centred-care <span>Best interests of child: looking at their interests broadly & not focusing exclusively on biomed facts; value judgment; harm-benefit balance Family centered-care: triadic model of therapeutic relationship; child’s best interest trumps FCC 9yo with HIV, parents do not want child to know Dx. Give 2 reasons to supp
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Highlight doc Day 1
ice Agree: 1) best interests of the child (non-maleficence, beneficence), 2) family centred-care Best interests of child: looking at their interests broadly & not focusing exclusively on biomed facts; value judgment; harm-benefit balance <span>Family centered-care: triadic model of therapeutic relationship; child’s best interest trumps FCC 9yo with HIV, parents do not want child to know Dx. Give 2 reasons to support parents, 2 reasons to support informing the child. How would this change if he was 12yo? 
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Highlight doc Day 1
inician may rely upon during times of dilemma (2 marks). PRO s : better-informed clinical decision CON s : AEs (HA, back pain, hemorrhage) Strategies: 1) go along, 2) do it, 3) better understand decision/share rationale <span>BEST INTERESTS OF THE CHILD: survival, harms/benefits, Tx, QoL DEVELOPING CHILD AUTONOMY FAMILY CENTRED CARE TRUTH TELLING/DISCLOSURE CONFIDENTIALITY: exceptions (harm, self-harm, abuse <16y) Resources: hospital ethicist, CCB (if concern over best interests) 14yo ♂ comes to you with whom it took time for you to develop trusting relationship. He confide
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Growth
GROWTH Failure to Thrive: cross 2 %-tiles, wt <3%-tile, <80% ideal body wt A 14yo ♂ with 1y Hx of FTT. He is pale and has diffuse abdominal pain. What are possible causes? What are 5 tests you would do to narrow your differential? &#
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Growth
GROWTH Failure to Thrive: cross 2 %-tiles, wt <3%-tile, <80% ideal body wt A 14yo ♂ with 1y Hx of FTT. He is pale and has diffuse abdominal pain. What are possible causes? What are 5 tests you would do to narrow your differential? DDx: non-organic, celiac, IBD, CF, T1DM, haematologic, malignancy, liver disease, obstructive uropathy Ix: CBC/Fe, celiac screen (tTGT), lytes, urea, Cr, TSH, U/A, Ca 2+ , Vit ADE 14yo at 3 rd %ile weight + 10 th %ile height is not eating well. What are 3 possible causes? See above A full term baby presents with an eating
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Growth
obstructive uropathy Ix: CBC/Fe, celiac screen (tTGT), lytes, urea, Cr, TSH, U/A, Ca 2+ , Vit ADE 14yo at 3 rd %ile weight + 10 th %ile height is not eating well. What are 3 possible causes? See above <span>A full term baby presents with an eating disorder (i.e. FTT). What is your DDx? ↓intake: non-organic , GERD, structural, CNS, genetic ↓absorption: CF, CMPA, short gut, biliary atresia, GI ↑loss: gastroenteritis ↑demand: cardiac, ↑THY, infection, respiratory Ineffective use: inborn error of metabolism Obesity 14yo ♂ with weight of 67 kg, height 150cm. Calculate BMI: 29.8 kg/m 2 4 complications of obesity: HTN, dyslipidemia, OSA, SCFE, nonEtO
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Growth
ganic , GERD, structural, CNS, genetic ↓absorption: CF, CMPA, short gut, biliary atresia, GI ↑loss: gastroenteritis ↑demand: cardiac, ↑THY, infection, respiratory Ineffective use: inborn error of metabolism Obesity <span>14yo ♂ with weight of 67 kg, height 150cm. Calculate BMI: 29.8 kg/m 2 4 complications of obesity: HTN, dyslipidemia, OSA, SCFE, nonEtOH fatty liver 3 tests to perform for obesity: lipids, GLUC, HbA1c, ALT/AST, liver U/S Newborn Growth Parameters&#
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Growth
esia, GI ↑loss: gastroenteritis ↑demand: cardiac, ↑THY, infection, respiratory Ineffective use: inborn error of metabolism Obesity 14yo ♂ with weight of 67 kg, height 150cm. Calculate BMI: 29.8 kg/m 2 <span>4 complications of obesity: HTN, dyslipidemia, OSA, SCFE, nonEtOH fatty liver 3 tests to perform for obesity: lipids, GLUC, HbA1c, ALT/AST, liver U/S Newborn Growth Parameters Weight • At birth = 3.0‐3.5kg (avg) • Normal to lose up to 10% of birth weight in first 4‐7 days o BUT should return to birth weight
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Growth
14yo ♂ with weight of 67 kg, height 150cm. Calculate BMI: 29.8 kg/m 2 4 complications of obesity: HTN, dyslipidemia, OSA, SCFE, nonEtOH fatty liver 3 tests to perform for obesity: lipids, GLUC, HbA1c, ALT/AST, liver U/S <span>Newborn Growth Parameters Weight • At birth = 3.0‐3.5kg (avg) • Normal to lose up to 10% of birth weight in first 4‐7 days o BUT should return to birth weight no later than 10‐14 days • Doubles birth weight by 4‐6 months; triples birth weight by 1 year • Quadruples birth weight by 2 years Head Circumference • At birth = 35cm (avg) o <32cm small head = small brain until proven otherwise • May be inaccurate at birth due to caput succedaneum, moldin
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Growth
mal to lose up to 10% of birth weight in first 4‐7 days o BUT should return to birth weight no later than 10‐14 days • Doubles birth weight by 4‐6 months; triples birth weight by 1 year • Quadruples birth weight by 2 years <span>Head Circumference • At birth = 35cm (avg) o <32cm small head = small brain until proven otherwise • May be inaccurate at birth due to caput succedaneum, molding • 0‐3mths = +2cm/mth • 3‐6mths =+1cm/mth • 6‐12mths = +0.5cm/mth Height • At birth = 50cm (avg) • Doubles height by 4 years • Measure recumbent length until 2 years, then standing height Normal Growth Velocity 
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Growth
• At birth = 35cm (avg) o <32cm small head = small brain until proven otherwise • May be inaccurate at birth due to caput succedaneum, molding • 0‐3mths = +2cm/mth • 3‐6mths =+1cm/mth • 6‐12mths = +0.5cm/mth <span>Height • At birth = 50cm (avg) • Doubles height by 4 years • Measure recumbent length until 2 years, then standing height Normal Growth Velocity Growth Charts • Critical to use gender and age appropriate growth charts • In 2010, the CPS, RCFPC and the Dieticians of Can
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Growth
, molding • 0‐3mths = +2cm/mth • 3‐6mths =+1cm/mth • 6‐12mths = +0.5cm/mth Height • At birth = 50cm (avg) • Doubles height by 4 years • Measure recumbent length until 2 years, then standing height <span>Normal Growth Velocity Growth Charts • Critical to use gender and age appropriate growth charts • In 2010, the CPS, RCFPC and the Dieticians of Canada, recommended the use of t
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Growth
the use of the 2006 WHO Growth Standards and Reference charts • WHO Growth Standards based on longitudinal data from solely breast fed for first six months, healthy children from diverse ethnic and geographic backgrounds; <span>use BMI after age 10. • Growth charts are also available for premature infants and certain syndromes • Use corrected age up to 2 years for plotting premature infants Failure to Thri
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Growth
om diverse ethnic and geographic backgrounds; use BMI after age 10. • Growth charts are also available for premature infants and certain syndromes • Use corrected age up to 2 years for plotting premature infants <span>Failure to Thrive Definition • Weight < 3%ile (the further below the curve the more likely to be pathologic in origin) • Weight falls across major %ile lines • Weight < 80% of ideal body weight* * use appropriate growth charts for gender and certain genetic conditions Factors Affecting Physical Growth • Genetics • Intrauterine factors • "Internal time clock" • Nutrition • Endocrine hormones • Chronic infec
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Growth
ther below the curve the more likely to be pathologic in origin) • Weight falls across major %ile lines • Weight < 80% of ideal body weight* * use appropriate growth charts for gender and certain genetic conditions <span>Factors Affecting Physical Growth • Genetics • Intrauterine factors • "Internal time clock" • Nutrition • Endocrine hormones • Chronic infections/diseases • Psychosocial factors Etiology • Inadequate intake: insufficient provision of food, vomiting, oro‐motor dysfunction • Inadequate absorption: pancreatic insufficiency, celiac disease
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Growth
onditions Factors Affecting Physical Growth • Genetics • Intrauterine factors • "Internal time clock" • Nutrition • Endocrine hormones • Chronic infections/diseases • Psychosocial factors <span>Etiology • Inadequate intake: insufficient provision of food, vomiting, oro‐motor dysfunction • Inadequate absorption: pancreatic insufficiency, celiac disease • Increased utilization: chronic diseases, hyperthyroidism • Ineffective utilization: chromosomal disorders • Increased losses: chronic diarrhea, urinary losses Differential Diagnosis Nonorganic/ Psychosocial Most common cause of FTT, often seen in conjunction with organic FTT Specific Organic Diseases • Genetic: T
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Growth
adequate absorption: pancreatic insufficiency, celiac disease • Increased utilization: chronic diseases, hyperthyroidism • Ineffective utilization: chromosomal disorders • Increased losses: chronic diarrhea, urinary losses <span>Differential Diagnosis Nonorganic/ Psychosocial Most common cause of FTT, often seen in conjunction with organic FTT Specific Organic Diseases • Genetic: Turner/Downs/Russell Silver Syndrome, FAS, TORCH • Cardiac: Chronic cardiac failure • Pulmonary: Recurrent or chronic infections, Cystic Fibrosis • GI: GERD, vomiting, IBD, chronic liver disease, malabsorption syndromes (Celiac Disease, CF, Schwachman Diamond syndrome) • Renal: Chronic renal failure, obstructive uropathies • Endocrine: Hyperthyroidism, hypopituitarism, DM‐1, DI • CNS: Difficulty coordinating swallow, MR, CP, Diencephalic Syndrome • Haematology: Chronic hematologic disorders, malignancies • Inflammatory/Immune: SLE, immunodeficiencies Risk Factors Child Factors • Premature, low birth weight • Feeding, sleep or elimination problems • Recurrent illness • Developmental delay Pare
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Growth
perthyroidism, hypopituitarism, DM‐1, DI • CNS: Difficulty coordinating swallow, MR, CP, Diencephalic Syndrome • Haematology: Chronic hematologic disorders, malignancies • Inflammatory/Immune: SLE, immunodeficiencies <span>Risk Factors Child Factors • Premature, low birth weight • Feeding, sleep or elimination problems • Recurrent illness • Developmental delay Parental Factors • Parents abused or neglected as children • Unwanted, unplanned pregnancy • Marital problems, single parent • Drugs/alcohol • Young inexperienced parents • Unwell/stressed parent • Poor follow‐up, uncooperative parents • Misconceptions of eating habits and nutrition Child and Parental Factors • Difficulty feeding, refusal to feed • Colic, sleep problems • Behavioural issues • Parent not able to recognize child’s needs and respond to child’s cues Environmental Factors • Low SES, unemployment • Lack of support, social isolation • Lack of access to consistent medical care History • Duration of problem, detailed dietary and feeding history, appetite, behavior before and after feeds, BM history, vomiting • Pregnancy, birth, birth
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Growth
issues • Parent not able to recognize child’s needs and respond to child’s cues Environmental Factors • Low SES, unemployment • Lack of support, social isolation • Lack of access to consistent medical care <span>History • Duration of problem, detailed dietary and feeding history, appetite, behavior before and after feeds, BM history, vomiting • Pregnancy, birth, birth weight, postpartum history, developmental history, growth patterns • Family patterns of growth including parental heights and age of puberty • Current illnesses, symptoms, past medical history • Family relationships, detailed social history • Assess child’s temperament, child‐parent interaction, feeding behaviour, parental psychosocial issues Physical Exam • Ht/Wt/HC‐ plot on growth chart; compare to prior values • HR, RR, BP • Complete general physical examination Investigations/Imaging • Use your history and physical exam to guide your choice of investigations • Consider investigations to look for etiology and investiga
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Growth
rament, child‐parent interaction, feeding behaviour, parental psychosocial issues Physical Exam • Ht/Wt/HC‐ plot on growth chart; compare to prior values • HR, RR, BP • Complete general physical examination <span>Investigations/Imaging • Use your history and physical exam to guide your choice of investigations • Consider investigations to look for etiology and investigations to assess for other deficiencies • CBC, lytes, urea, creatinine, TSH, T4, U/A, celiac screen, vitamin A,D,E, ferritin, calcium • Consider karyotype, microarray, bone age (AP x‐ray of L hand and wrist) if also short stature Management • Treat underlying cause • Provide education about age‐appropriate foods, mealtime scheduling and behaviour • Caloric fortification of food • May need referral to dietitian, social work Overweight and Obesity Introduction • Growth monitoring should be performed at primary care visits for children and youth ages 17 and younger • BMI = mass
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Development
DEVELOPMENT [See chart] NORMAL Case on child not toilet training: what is the likely reason? Not yet interested in learning how, i.e. few signs present (requires physiologic, communication, psychologic) 5yo has been developing normally, but his father has been concerned he's been showing poor speech. What's the first Ix to do? MCQ: audiology testing, NOT genet
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Development
ee chart] NORMAL Case on child not toilet training: what is the likely reason? Not yet interested in learning how, i.e. few signs present (requires physiologic, communication, psychologic) <span>5yo has been developing normally, but his father has been concerned he's been showing poor speech. What's the first Ix to do? MCQ: audiology testing, NOT genetic testing Developmental milestones for 6mo. Normal: tripod sits, pivots in prone position, reaches/grasps objects, brings toy to mouth, babbles, squeals when excited, g
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Development
ogic, communication, psychologic) 5yo has been developing normally, but his father has been concerned he's been showing poor speech. What's the first Ix to do? MCQ: audiology testing, NOT genetic testing <span>Developmental milestones for 6mo. Normal: tripod sits, pivots in prone position, reaches/grasps objects, brings toy to mouth, babbles, squeals when excited, grunts in anger, stranger anxiety starts Lists developmental progress for a 12mo, what type of delay does this child have - language, fine motor, gross motor, or global delay? Normal: gets into sitti
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Development
ting Developmental milestones for 6mo. Normal: tripod sits, pivots in prone position, reaches/grasps objects, brings toy to mouth, babbles, squeals when excited, grunts in anger, stranger anxiety starts <span>Lists developmental progress for a 12mo, what type of delay does this child have - language, fine motor, gross motor, or global delay? Normal: gets into sitting position without help, stands without support, walks while holding on, neat pincer grasp, places cubes in cup with release, releases ball with throw, says 2-3 words, understand simple requests and questions, uses facial expressions/actions/sounds to make needs known, responds to own name, separation anxiety begins 3 yo development milestone (circle 8): I guess the biggest lesson I took away with me from this exam is from the key features section and this question in particular: list
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Development
sp, places cubes in cup with release, releases ball with throw, says 2-3 words, understand simple requests and questions, uses facial expressions/actions/sounds to make needs known, responds to own name, separation anxiety begins <span>3 yo development milestone (circle 8): I guess the biggest lesson I took away with me from this exam is from the key features section and this question in particular: listen to what your predecessors have to say about the exam in the past exams you see in this email account! When I saw, in one of the previous peds exam, that one is required to pick things out of a list of 20 development milestones, none of which appears in Toronto Notes, I did not take the warning seriously, and I'm forced to pay for my irreverence. I randomly circled 8 things and would be lucky if I can walk away with half the marks. So the lesson is that not only should you remember the short list of developmental milestones from Toronto Notes or the Peds handbook you got from year 2 for the short answers part, but you should also remember a longer, more exhaustive list of milestones from some other source for the key features version of the development milestonesànot true in 2015 Normal: walks upstairs using handrail, stands on one foot, rides tricycles, stacks 10 blocks, twists lid off jars, copies a circle, combines 5 or more words in a sentence, understands 2-3 step commands, recognizes colours, shares willingly some of the time, make-believe games, plays with others, listens to music or stories for 5-10 minutes, jumping on one foot, washes and dries own hands, dresses self independently except shoe laces, knows own sex, tells detailed stories, knows primary colours, speaks with plurals Pick developmental milestones from a list (I think for a 3yo and another one for a 4yo?) See above Developmental Milestones achieved by 15 mo? 18m
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Development
milestones from a list (I think for a 3yo and another one for a 4yo?) See above Developmental Milestones achieved by 15 mo? 18mo? What about 6-10 yrs? 16 wks? See chart Developmental Milestones <span>There are four main areas of developement – gross motor, fine motor, language and social. All areas should be explored when exploring a developmental history. The milestones cited are, on average, those at the 50th percentile for age. Develo
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Development
out 6-10 yrs? 16 wks? See chart Developmental Milestones There are four main areas of developement – gross motor, fine motor, language and social. All areas should be explored when exploring a developmental history. <span>The milestones cited are, on average, those at the 50th percentile for age. Developmental Problems Differential Diagnosis • Motor o Problems with CNS (e.g., Cerebral palsy) o Problems with PNS (e.g., Muscul
Flashcard 1473379962124
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itRome had begun expanding shortly after the founding of the republic in the 6th century BC
Original toplevel document
Roman Empire - Wikipediagelink] [emptylink] The Augustus of Prima Porta (early 1st century AD) [imagelink] [emptylink] Bust of Tiberius Julius Sauromates II (d. 210 AD), ruler of the Bosporan Kingdom in Roman Crimea, one of Rome's client states <span>Rome had begun expanding shortly after the founding of the republic in the 6th century BC, though it did not expand outside the Italian Peninsula until the 3rd century BC. Then, it was an "empire" long before it had an emperor. [10] [11] [12] [13] The Roman Republ
Flashcard 1473382321420
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itRome had begun expanding shortly after the founding of the republic in the 6th century BC
Original toplevel document
Roman Empire - Wikipediagelink] [emptylink] The Augustus of Prima Porta (early 1st century AD) [imagelink] [emptylink] Bust of Tiberius Julius Sauromates II (d. 210 AD), ruler of the Bosporan Kingdom in Roman Crimea, one of Rome's client states <span>Rome had begun expanding shortly after the founding of the republic in the 6th century BC, though it did not expand outside the Italian Peninsula until the 3rd century BC. Then, it was an "empire" long before it had an emperor. [10] [11] [12] [13] The Roman Republ
Flashcard 1473384680716
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itRome had begun expanding shortly after the founding of the republic in the 6th century BC
Original toplevel document
Roman Empire - Wikipediagelink] [emptylink] The Augustus of Prima Porta (early 1st century AD) [imagelink] [emptylink] Bust of Tiberius Julius Sauromates II (d. 210 AD), ruler of the Bosporan Kingdom in Roman Crimea, one of Rome's client states <span>Rome had begun expanding shortly after the founding of the republic in the 6th century BC, though it did not expand outside the Italian Peninsula until the 3rd century BC. Then, it was an "empire" long before it had an emperor. [10] [11] [12] [13] The Roman Republ
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Development
e motor, language and social. All areas should be explored when exploring a developmental history. The milestones cited are, on average, those at the 50th percentile for age. Developmental Problems <span>Differential Diagnosis • Motor o Problems with CNS (e.g., Cerebral palsy) o Problems with PNS (e.g., Muscular dystrophy) o Metabolic conditions (e.g., Hypothyroidism) o Genetic syndromes (e.g., Down Syndrome) • Language o Structural/functional abnormalities of oromotor anatomy o Hearing impairment o Pure language disorders o Pervasive developmental disorders (e.g., Autism Spectrum Disorder) • Cognitive o Global developmental delay due to: - Genetic conditions (e.g., Fragile X) - Deprived environment - Prenatal/perinatal events leading to brain anoxia/ischemia (rare) - Prenatal exposures (e.g., Fetal Alcohol Spectrum Disorders) • Emotional/Social o Pervasive developmental disorders (e.g., Autism Spectrum Disorder) o Deprived environment Management • Motor o Educate parents about poor correlation between motor delays and intelligence o Refer to Physiotherapy and Occupational therapy o
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Development
brain anoxia/ischemia (rare) - Prenatal exposures (e.g., Fetal Alcohol Spectrum Disorders) • Emotional/Social o Pervasive developmental disorders (e.g., Autism Spectrum Disorder) o Deprived environment <span>Management • Motor o Educate parents about poor correlation between motor delays and intelligence o Refer to Physiotherapy and Occupational therapy o Educate parents on developmental targets and techniques for helping achieve specific milestones - e.g. adequate ‘Tummy Time’ to facilitate development of head control, rolling over, etc. • Language o Audiology assessment o Referral to local early intervention services o Speech and language (SLP) evaluation o Enroll child in nursery school o Educate parents regarding language facilitation techniques - make noises or sing and repeat sounds the child says - ask questions/make comments that lead to a response - label objects and emphasize action words - read to the child - use simple, slow language • Cognitive o Thorough history: - Pregnancy (obstetrical history, exposures, complications) - Birth (gestational age, complications, delivery, resuscitation) - Family History (parents, siblings, consanguinity) - Social History (identify deprived environments) o Physical exam including head growth, dysmorphic features, neurologic exam o Hearing/vision assessment o Other tests as indicated: karyotype, blood lead levels, metabolic screen, TSH, CT/MRI o Find appropriate schooling/community living o Help family find support groups, funding, respite • Emotional/Social o Early intervention with early intervention therapists o Provide opportunities for increased contact with other children e.g., play groups, structured daycare o Refer to specific therapeutic groups o If applicable, remove child from deprived environment with help of children’s aid society Developmental Surveillance Rourke Baby Record Available in the Syllabus and through the CPS website at: www.cps.ca/english/statements/CP/Rourke/RBROntario.pdf&
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Development
: o Growth and nutrition o Nutrition o Development milestones – to aid developmental surveillance, not a screen. Set after time of normal milestone acquisition. o Anticipatory guidance o Physical examination <span>Enhanced 18Month WellBaby Visit Syllabus: Canadian Task Force on Preventative Health Care. Recommendations on screening for developmental delay. CMAJ. 2016; 188(8):579. • Important time to review child’s developmental domains and achievement of milestones • Visit should incorporate use of Rourke Baby Record, screening for parental morbidities (mental health, physical illness), promotion of literacy activities (reading, singing), and information about resources • Standard developmental screening tools (eg: Nipissing) no longer recommended for children whose parents or clinicians have no concerns regarding delay • Screening still appropriate in children presenting with signs/symptoms, or parental concerns of delay. Greig Health Record Available in the Syllabus and through the CPS website at: www.cps.ca/english/statements/CP/PreventiveCare.htm • Evidenced based health prom
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Development
BMI o Psychosocial history and development o Nutrition o Education o Behaviour and family issues o Injury prevention and safety o Physical examination o Guidelines and resources (eg: vaccinations) <span>Attention Deficit/Hyperactivity Disorder Syllabus: Floet et al. Attention Deficit/Hyperactivity Disorder. Pediatrics in Review. 2010;31(2):56. American Academy of Pediatrics. ADHD: Clinical Practice Guideline for the Diagnosis, Evaluation and Treatment of Attention‐Deficit/Hyperactivty Disorder in Children and Adolescents. Pediatrics. 2011;128(5):1007. Introduction • ADHD is a neurobehavioral disorder defined by symptoms of inattention, hyperactivity, and impulsivity. • There is a two‐ to three‐fold higher prevalence in boys than girls with girls being more likely to be diagnosed with the inattentive‐type ADHD • Can profoundly effect academic performance, social interactions and well being DSM5 Diagnostic Criteria for Attention Deficit/Hyperactivity Disorder A. A persistent pattern of inattention and/or hyperactivity‐impulsivity that interferes with functioning or development, as characterized by (1) and/or (2): 1. Inattention: Six (or more) of the following symptoms have persisted for at least 6 months to a degree that is inconsistent with developmental level and that negatively impacts directly on social and academic/occupational activities: a. Often fails to give close attention to details or makes careless mistakes in schoolwork, at work, or during other activities (e.g., overlooks or misses details, work is inaccurate). b. Often has difficulty sustaining attention in tasks or play activities (e.g., has difficulty remaining focused during lectures, conversations, or lengthy reading). c. Often does not seem to listen when spoken to directly (e.g., mind seems elsewhere, even in the absence of any obvious distraction). d. Often does not follow through on instructions and fails to finish schoolwork, chores, or duties in the workplace (e.g., starts tasks but quickly loses focus and is easily sidetracked). e. Often has difficulty organizing tasks and activities (e.g., difficulty managing sequential tasks; difficulty keeping materials and belongings in order; messy, disorganized work; has poor time management; fails to meet deadlines). f. Often avoids, dislikes, or is reluctant to engage in tasks that require sustained mental effort (e.g., schoolwork or homework; for older adolescents, preparing reports, completing forms, reviewing lengthy papers). g. Often loses things necessary for tasks or activities (e.g., school materials, pencils, books, tools, wallets, keys, paperwork, eyeglasses, mobile telephones). h. Is often easily distracted by extraneous stimuli (for older adolescents, may include unrelated thoughts). i. Is often forgetful in daily activities (e.g., doing chores, running errands; for older adolescents, returning calls, paying bills, keeping appointments). j. Hyperactivity and impulsivity: Six (or more) of the following symptoms have persisted for at least 6 months to a degree that is inconsistent with developmental level and that negatively impacts directly on social and academic/occupational activities: a. Often fidgets with or taps hands or feet or squirms in seat. b. Often leaves seat in situations when remaining seated is expected (e.g., leaves his or her place in the classroom, in the office or other workplace, or in other situations that require remaining in place). c. Often runs about or climbs in situations where it is inappropriate. (Note: In adolescents, may be limited to feeling restless.) d. Often unable to play or engage in leisure activities quietly. e. Is often "on the go," acting as if "driven by a motor" (e.g., is unable to be or uncomfortable being still for extended time, as in restaurants, meetings; may be experienced by others as being restless or difficult to keep up with). f. Often talks excessively. g. Often blurts out an answer before a question has been completed (e.g., completes people's sentences; cannot wait for turn in conversation). h. Often has difficulty waiting his or her turn (e.g., while waiting in line). i. Often interrupts or intrudes on others (e.g., butts into conversations, games, or activities; may start using other people's things without asking or receiving permission; for adolescents, may intrude into or take over what others are doing). B. Several inattentive or hyperactive‐impulsive symptoms were present prior to age 12 years. C. Several inattentive or hyperactive‐impulsive symptoms are present in two or more settings (e.g., at home, school, or work; with friends or relatives; in other activities). D. There is clear evidence that the symptoms interfere with, or reduce the quality of, social, academic, or occupational functioning. E. The symptoms do not occur exclusively during the course of schizophrenia or another psychotic disorder and are not better explained by another mental disorder (e.g., mood disorder, anxiety disorder, dissociative disorder, personality disorder, substance intoxication or withdrawal). Types • Combined presentation: If both Criterion A1 (inattention) and Criterion A2 (hyperactivity‐impulsivity) are met for the past 6 months. • Predominantly inattentive presentation: If Criterion A1 (inattention) is met but Criterion A2 (hyperactivity‐impulsivity) is not met for the past 6 months. • Predominantly hyperactive/impulsive presentation: If Criterion A2 (hyperactivity‐impulsivity) is met and Criterion A1 (inattention) is not met for the past 6 months. Risk Factors • Genetic factors: heritability is approximately 75% • Nongenetic factors: perinatal stress and low birth weight, traumatic brain injury, maternal smoking during pregnancy, severe early deprivation Physical Exam A physical examination is important in ruling out underlying medical or developmental problems such as the following: • emotional or behavioral (eg. anxiety, depression, oppositional defiant and conduct disorders) • developmental (eg. learning and language disorders or other neurodevelopmental disorders) • physical conditions (eg. tics, sleep apnea) Examination should include observation of the child and the parent and their relationship. Investigations • Laboratory and imaging studies are not routinely recommended. However, consideration of hearing and vision tests, thyroid function studies, blood lead levels, genetic karyotyping and brain imaging studies if indicated by past medical history or physical examination • In most cases, laboratory investigations will not be necessary • Consider a psycho‐educational evaluation including both cognitive and academic testing to assess for learning problems Management Syllabus: Belanger et al. Cardiac risk assessment before the use of stimulant medications in children and youth. Paediatrics and Child Health. 2009;14(9):579. Feldman et al. Extended‐release medications for children and adolescents with attention‐deficit hyperactivity disorder. Paediatrics and Child Health. 2009;14(9):593. Bernard‐Bonnin A‐C et al. The use of alternative therapies in treating children with attention deficit hyperactivity disorder. Paediatrics and Child Health. 2002;7(10):710zXXZas Paediatrics and Child Health. 2009;14(9):593.F. • Approach to treatment is multidisciplinary • Psychoeducation and support for patient and family • In cases of ADHD without co‐morbidity, behavioural therapies have not been shown to be helpful for the core symptoms of ADHD • School aged children (6‐18 yrs): o First line is stimulant medication(s) o Second line is non‐stimulant medications o Third line is behavior management: positive reinforcement, time out, response cost, token economy • Pre‐school aged children (4‐5 yrs): o First line is behavior management: positive reinforcement, time out, response cost, and token economy o Second line is stimulant medication(s) • Dietary interventions such as the elimination of sugar have NOT proven to have an observable effect. Other dietary interventions (i.e., elimination of food additives or addition of dietary supplements) require evidence‐based research • Follow‐up and long‐term management are required as ADHD does not resolve with age Medications • Stimulants (methylphenidate, dextroamphetamine) are considered first line because they are highly efficacious in reducing symptoms • Extended release stimulant medications are associated with decreased use of street drugs among adolescents with ADHD, decrease in rate of injuries, STI’s and unwanted pregnancies • Immediate‐release medications such as Ritalin should be avoided as they are much easier to divert, crushed Ritalin may be snorted or made into an injectible form, mixed with narcotics and taken as a ‘speed‐ball’ • Medications should be used 365 days per year in adolescents • Careful titration of medication to optimize effects, minimize side effects and enhance compliance is essential. Autism Spectrum Disorder Syllabus: Johnson C et al. Identification and Evaluation of Chidlren with Autism Spectrum Disorders. Pediatrics. 2007;120(5):1183. Har
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Development
th narcotics and taken as a ‘speed‐ball’ • Medications should be used 365 days per year in adolescents • Careful titration of medication to optimize effects, minimize side effects and enhance compliance is essential. <span>Autism Spectrum Disorder Syllabus: Johnson C et al. Identification and Evaluation of Chidlren with Autism Spectrum Disorders. Pediatrics. 2007;120(5):1183. Harrington et al. The Clinician’s Guide to Autism. Pediatrics in Review. 2014;35(2):62. Simms et al. Autism, Language Disorder, and Social (Pragmatic) Communication Disorder: DSM‐V and Diferential Diagnosis. Pediatrics in Review. 2015;36(8):355. Introduction • The essential features of autism spectrum disorder are persistent impairment in reciprocal social communication and social interaction, and restricted, repetitive patterns of behavior, interests, or activities. • These symptoms are present from early childhood and limit or impair everyday functioning • Social skills deficits can be noticed in infancy with aversion to cuddling and lack of acknowledgement of the caregiver • Also can involve language delays/deficits, motor signs (e.g., stereotypies, toe walking), sensory deficits (e.g., intolerance to sound) • Cognitive abilities vary; typically difficulties with reasoning/planning, greater abilities in rote memory DSM5 Criteria for Autism Spectrum Disorder A. Persistent deficits in social communication and social interaction across multiple contexts, as manifested by the following, currently or by history (examples are illustrative, not exhaustive; see text): 1. Deficits in social‐emotional reciprocity, ranging, for example, from abnormal social approach and failure of normal back‐and‐forth conversation; to reduced sharing of interests, emotions, or affect; to failure to initiate or respond to social interactions. 2. Deficits in nonverbal communicative behaviors used for social interaction, ranging, for example, from poorly integrated verbal and nonverbal communication; to abnormalities in eye contact and body language or deficits in understanding and use of gestures; to a total lack of facial expressions and nonverbal communication. 3. Deficits in developing, maintaining, and understanding relationships, ranging, for example, from difficulties adjusting behavior to suit various social contexts; to difficulties in sharing imaginative play or in making friends; to absence of interest in peers. B. Restricted, repetitive patterns of behavior, interests, or activities, as manifested by at least two of the following, currently or by history (examples are illustrative, not exhaustive; see text): 1. Stereotyped or repetitive motor movements, use of objects, or speech (e.g., simple motor stereotypies, lining up toys or flipping objects, echolalia, idiosyncratic phrases). 2. Insistence on sameness, inflexible adherence to routines, or ritualized patterns of verbal or nonverbal behavior (e.g., extreme distress at small changes, difficulties with transitions, rigid thinking patterns, greeting rituals, need to take same route or eat same food every day). 3. Highly restricted, fixated interests that are abnormal in intensity or focus (e.g., strong attachment to or preoccupation with unusual objects, excessively circumscribed or perseverative interests). 4. Hyper‐ or hyporeactivity to sensory input or unusual interest in sensory aspects of the environment (e.g., apparent indifference to pain/temperature, adverse response to specific sounds or textures, excessive smelling or touching of objects, visual fascination with lights or movement). C. Symptoms must be present in the early developmental period (but may not become fully manifest until social demands exceed limited capacities, or may be masked by learned strategies in later life). D. Symptoms cause clinically significant impairment in social, occupational, or other important areas of current functioning. E. These disturbances are not better explained by intellectual disability (intellectual developmental disorder) or global developmental delay. Intellectual disability and autism spectrum disorder frequently cooccur; to make comorbid diagnoses of autism spectrum disorder and intellectual disability, social communication should be below that expected for general developmental level. Risk Factors • Male (4x risk) • Having another child with autism • Advanced parental age • Genetic/cytogenetic/syndromic conditions o Down Syndrome, Tuberous sclerosis, untreated PKU, Fragile X, Angelman, Cornelia de Lange syndrome • Early bilateral mesial temporal lobe lesions due to herpes simplex or anoxic/ischemic damage • Very low birth weight, especially with retinopathy of prematurity • No association between MMR vaccination and autism o Studies that showed causation were fraudulent Screening • Developmental surveillance is encouraged at all well baby/child visits • Developmental screening at 18 month visit • Targeted (secondary) screening is recommended in high risk children (risk factors, parental concerns, teacher observations, missed milestones etc) and requires use of specific screening tools (e.g. CHAT) • Determination that a child is at high risk of ASD should result in immediate referral to an experienced diagnostician or an interdisciplinary assessment team INADEQUATE LANGUAGE FEATURES SUGGESTING AUTISM At any age • Regression of language or communicative gestures • Lack of reliable orienting to speech, turning to name • Concern about language comprehension • Persistent mutism unpredictably interrupted by rare isolated clear words or sentences In toddlers • No pointing by 1 year; dragging by the hand • No words by 12‐14 months • Less than a dozen words by 18 months • No 2‐word phrases by 2 years or sentences by 3 years • Very delayed or absent head shaking or nodding to signify no/yes In preschoolers and older children • Failure to answer questions or responding beside the point • Inability to use language conversationally, “talking to talk” rather than to communicate (request, show, etc) • Frequent, persistent verbatim repetition (echolalia) • Persistent pronoun inversion (you/me confusion), referring to self by name • Verbatim repetition of overlearned expressions (delayed echolalia, formulaic speech) rather than self‐generated expressions • Inability to recount an event or tell a coherent story • Perseveration on a favorite topic • Overuse of pedantic words or expressions • High‐pitched, sing‐song, or uninflected robotic speech Investigations • Formal audiological assessment o Consider blood tests: genetic (karyotype, Fragile X, 22q deletion, microarray), metabolic, lead levels and neurologic tests: MRI, EEG Diagnosis • In accordance with DSM‐V Criteria • Interdisciplinary approach is ideal • Assessment of cognitive and developmental levels is required • Can be diagnosed as early as 18 months by experienced professionals • Should be made on the basis of a thorough developmental history and structured behavioural observation and clinical judgment. • The use of at least one standardized, norm‐referenced parent report measure and at least one standardized, norm‐referenced behavioral observation measure is recommended. Management • Early, multi‐disciplinary intervention is beneficial • Structured learning • Speech and language assessment and therapy • Occupational therapy ‐ sensory integration • Behaviour management support • Medications for self‐injurious and aggressive behaviours o SSRIs, psychotropic drugs (e.g., Risperidone), anticonvulsants • Social skills training • Vocational counseling Note: Elimination diets and vitamins have no proven efficacy Learning Disorders Syllabus: Rimrodt et al. Learning Disabilities and School Failure. Pediatrics in Review. 2011;32(8):315. Byrd R. School Failure: Assessment,
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Development
‐injurious and aggressive behaviours o SSRIs, psychotropic drugs (e.g., Risperidone), anticonvulsants • Social skills training • Vocational counseling Note: Elimination diets and vitamins have no proven efficacy <span>Learning Disorders Syllabus: Rimrodt et al. Learning Disabilities and School Failure. Pediatrics in Review. 2011;32(8):315. Byrd R. School Failure: Assessment, Intervention, and Prevention in Primary Care Pediatrics. Pediatrics in Review. 2005;26(7):233. • Represent a disability based on a descrepency between a person’s intellectual ability and actual academic performance • Further specificed into the particular area of academic function affected: o Mathematics disorder o Reading disorder o Disorder of reading expression • Any child who has school problems and is suspected of having a learning disability should be referred for a comprehensive psychoeducational evaluation • Accomodations can be made at school through the Identification, Placement, and Review Committee (IPRC). The IPRC will: o decide whether or not a student should be identified as exceptional o identify the areas of a student’s exceptionality o decide an appropriate placement for a student o review identification and placement at least once per school year • An IEP (Individual Education Plan) is developed (in consultation with parents and the student) for each student who has been identified as exceptional by the IPRC process. An IEP is a written plan that describes the strengths and needs of the student, services established to meet that student’s needs, and how these should be delivered Bullying Syllabus: Lamb et al. Approach to Bullying and Victimization. Canadian Family Physician. 2009;55(4):356. Introduction • Defined as the use of pow
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Development
been identified as exceptional by the IPRC process. An IEP is a written plan that describes the strengths and needs of the student, services established to meet that student’s needs, and how these should be delivered <span>Bullying Syllabus: Lamb et al. Approach to Bullying and Victimization. Canadian Family Physician. 2009;55(4):356. Introduction • Defined as the use of power or aggression to cause distress or control of another • Can be direct (face‐to‐face) or indirect (gossip, exclusion) • Negative actions can include: o Physical actions (punching, kicking, biting) o Verbal actions (threats, name calling, insults) o Social exclusion (spreading rumours, gossiping, excluding) • Actions are repeated and the intensity or duration establishes dominance History • When a physician identifies a possible bullying situation, the following questions can help determine what type of help may be appropriate o Who do you bully/who bullys you? o What do you do to others/what do others do to you? (e.g. gossiping, insults, hitting, etc.) o When and how often do you bully/are you bullied? o Where do you bully/where are you bullied? o Why do you bully others/why do you think you are bullied? o How do you think the kids feel when you bully them or how do you feel when you are bullied? Management • Comprehensive strategies that encompass the school, family and community are most likely to be effective o establish a social school environment that promotes safety o provide access to health and mental health services o integrate school, family and community prevention efforts o provide training to enable school staff to promote safety and prevent violence effectively Toilet Training Syllabus: Clifford et al. Toilet Learning: Anticipatory Guidance with a child‐oriented approach. Paediatrics and Child Health. 2000;5(6):333. F
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Development
fety o provide access to health and mental health services o integrate school, family and community prevention efforts o provide training to enable school staff to promote safety and prevent violence effectively <span>Toilet Training Syllabus: Clifford et al. Toilet Learning: Anticipatory Guidance with a child‐oriented approach. Paediatrics and Child Health. 2000;5(6):333. Feldman. Managing primary nocturnal enuresis. Paediatr Child Health. 2005; 10(10):611. Bayne et al. Nocturnal enuresis: An approach to assessment and treatment. Peditrics in review. Pediatrics in Review. 2014; 35(8):327. Austin et al. Dysfunctional Voiding. Pediatrics in Review. 2000;21(10):336. Har et al. Encoperesis. Pediatrics in Review. 2010;31(9):368. Signs of a child’s toilet learning readiness • Can understand and follow simple instruction • Diaper is consistently dry for 2 to 3 hours at a time or after naps • Bowel movements are somewhat regular and predictable • Seems uncomfortable with soiled diapers and wants to be changed • Recognizes and tells or shows need to urinate or stool • Can walk to bathroom and pull pants up and down • Is stable on potty (good trunk support) • Interested and motivated to learn how to use the potty • Shows interest in 'big kid' underwear - Child does not need to show all of the signs, but at least a few should be present to indicate the child is ready for toilet training - Average age for a child to be toilet trained is between 2 to 3 years old - Advise parents to expect accidents during initial training Sleep Requirements Newborns • Should sleep on back in crib with flat surface, no pillows or soft items • In parents’ room for first 6 months Older b
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Development
least a few should be present to indicate the child is ready for toilet training - Average age for a child to be toilet trained is between 2 to 3 years old - Advise parents to expect accidents during initial training <span>Sleep Requirements Newborns • Should sleep on back in crib with flat surface, no pillows or soft items • In parents’ room for first 6 months Older babies • Maintain regular daytime and bedtime schedule • Start consistent bedtime routine • Avoid putting baby to bed with a bottle Sleep Problems Night terrors • Parasomnia that occurs in first third of night • High to extreme autonomic agitation • High arousal threshold, agitated if awakened • No daytime sleepiness or recall of event Nightmares • Occur in last third of night during REM sleep • Mild to high autonomic arousal/agitation • Low arousal threshold, agitated after event • Can have daytime sleepiness and frequent, vivid recall of event • Very common BEARS Screening Tool for Pediatric Sleep Disorders Sleep associations • Infant or toddler child has learned to fall asleep only under certain conditions or has specific sleep associations that require parental intervention, such as being rocked or fed, which are usually readily available at bedtime • During the night, when the infant or toddler awakens, they are not able to get back to sleep ("self‐soothe") unless those same conditions are available 90 o The infant then "signals" the caregiver by crying or coming into the parents' bedroom if the child is no longer in a crib until the necessary associations are provided o Ferber method advocates that at bedtime child is put in bed while they are drowsy, but still awake, to help them learn how to fall asleep on their own (self‐soothe) Colic Syllabus: Cohen et al. Colic. Pediatrics in Review. 2012;33(7):332. • Infantile colic is defined as o paroxysms of irritability, fussiness or crying that
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Development
ntil the necessary associations are provided o Ferber method advocates that at bedtime child is put in bed while they are drowsy, but still awake, to help them learn how to fall asleep on their own (self‐soothe) <span>Colic Syllabus: Cohen et al. Colic. Pediatrics in Review. 2012;33(7):332. • Infantile colic is defined as o paroxysms of irritability, fussiness or crying that start and stop without obvious cause; o episodes lasting 3 h or more per day and occurring at least three days per week for at least three weeks; and o no failure to thrive • Peaks at 6 weeks of age and typically ends by 3‐4 months • Crying is most frequent in the late afternoon or evening • Holding or rocking and offering a pacifier might help • There is no evidence that medicines really help with colic • There is no or insufficient evidence to support dietary changes including probiotics, lactose free diet, soy formulas • If there is a concern about cow’s milk protein allergy, a time limited (two week) trial of hypoallergenic formula or elimination of cow’s milk from the maternal diet can be undertaken Gotta Find Strong Coffee Soon •Gross Motor •Fine Motor •Speech/ Language •Cognitive •Social Emotional, Behaviour •(Adaptive Skills) A
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Development
actose free diet, soy formulas • If there is a concern about cow’s milk protein allergy, a time limited (two week) trial of hypoallergenic formula or elimination of cow’s milk from the maternal diet can be undertaken <span>Gotta Find Strong Coffee Soon •Gross Motor •Fine Motor •Speech/ Language •Cognitive •Social Emotional, Behaviour •(Adaptive Skills) Approach to Developmental History -History of presenting illness -Perinatal history (TORCH inf's) -Past medical history -Hearing, vision, sleep, feeding&#
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Development
f cow’s milk from the maternal diet can be undertaken Gotta Find Strong Coffee Soon •Gross Motor •Fine Motor •Speech/ Language •Cognitive •Social Emotional, Behaviour •(Adaptive Skills) <span>Approach to Developmental History -History of presenting illness -Perinatal history (TORCH inf's) -Past medical history -Hearing, vision, sleep, feeding -Developmental history (-start asking from several age groups lower than current age; observe child) -Family history (developmental delay, learning disabilities metabolic/genetic conditions consanguinity) -Social history (typical day, language spoken at home, other children at home, daycare/preschool, child maltx/CAS, income, etc) physical exam •Weight, height and head circumference at 50th percentile (want to know if macro/microcephaly, any dysmoprhic ft's make sure to undress & look at skin) •Low, posteriorly rotated ears but no other dysmorphic features or unusual birth marks •Normal general and neurologic examinations GLOBAL DEVELOPMENTAL DELAY Significant delay (at least two standard deviations below the mean with standardized tests) in at least two developmental domains from the following: Gross or fine motor Speech/ language Cognition Social/ personal Activities of Daily Living -Child must be less than 5 years old Causes of GDD/ID . Pediatric milestones in development 1 year: - single words 2 years: - 2 word sentences -understands 2 step commands 3 years:
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Development
lopmental domains from the following: Gross or fine motor Speech/ language Cognition Social/ personal Activities of Daily Living -Child must be less than 5 years old Causes of GDD/ID . <span>Pediatric milestones in development 1 year: - single words 2 years: - 2 word sentences -understands 2 step commands 3 years: - 3 word combos -repeats 3 digits -rides tri cycle 4 years: -draws square -counts 4 objects Stairs mnemonic. Two at two. One at four. Two feet on each step at two years. One foot per step at four years. Birth to 1 Year: Remember that the goal of the first year is to be able to walk (walk at 12 months). At six months you are halfway there (remember “sit at six”). Just with th
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Development
-repeats 3 digits -rides tri cycle 4 years: -draws square -counts 4 objects Stairs mnemonic. Two at two. One at four. Two feet on each step at two years. One foot per step at four years. <span>Birth to 1 Year: Remember that the goal of the first year is to be able to walk (walk at 12 months). At six months you are halfway there (remember “sit at six”). Just with these two milestones you can pretty much fill in everything else. Remember that everything is from head to toe. So 2 months (the first time we really check milestones) you check for head lifting (neck control). You roll at 4 months (at level of shoulders and chest). Then, again, at six you sit. You crawl at 9 months and pull to stand (crawl, pull to stand at 9 months) which makes sense as being between sitting and walking. In Review: 2 months: lift head 45 degrees 4 months: roll over (front to back first, then back to front, easier if you can push off with hands) 6 months: sit (halfway to goal, halfway through year, “sit at six”) 9 months: crawl, stand (halfway between sitting and goal) 12 months: walk (the goal) 15 months – 5 years: Memorize these milestones in a story as they are harder to associate with particular months like the first year. Using this progression story may help you. 15 months: walks well 18 months: throws objects 24 months/2 years: up and down stairs (one foot at a time); run 3 years: Tricycle (3 wheels, 3 years), jump in place 4 years: up and down stairs alternating feet (2 feet x up/down = 4), balance on 1 foot for 4 seconds (legs look like a 4 when on 1 foot), hop 5 years: skip (5 looks like an “S”kips) Story: a child on the 1st floor of her house sits up, crawls, cruises, then 1) WALKS to stairs, 1.5) THROWS object up stairs, 2) CLIMBS up the stairs and RUNS to his trike, 3) RIDES a trike upstairs, JUMPS off, 4) RUNS down the stairs, HOPS off the stairs and 5) SKIPS away 3. Once you’ve memorized the months of well child checks and corresponding gross motor milestones, begin to memorize the archetype babies for each age group. These little stories incorporate all the other milestones into a single image which is much easier than trying to memorize many unrelated facts. There are some ways to conceptually link milestones across categories, but they are not frequent enough to be useful for fast recall and the salient milestones and timing which is what happens on tests and during morning report. Here are all the babies with milestones listed: 2 months: lift head 45 degrees (when laying on face), turns to sound, follows objects past midline, social smile Parent’s Little Baby: looks up to sound, smiles because he sees both his parents, one on either side of midline 4 months: lift head 90 degrees/raise up to chest, roll over, find midline, reach for objects, puts objects in mouth, coos (these are vowel sounds), and laughs Fat Happy Baby: baby is rolling and laughing and cooing because he just discovered midline and is reaching for cake that he will cram into his mouth 6 months: sit up with no head lag, raking grasp, transfer objects between hands, babbles (consonants), recognizes familiar faces Street-Corner Baby: sitting up on sidewalk, transferring a rake from hand to hand while babbling at people he thinks he recognizes 9 months: Crawl, pull to stand, point, specific babbling (mama, dada), stranger anxiety Watch Dog Baby: crawls to window, pulls to stand to see out, points at stranger in yard and says “mama” to get attention of parents. 12 months: Walk, pincer grasp, 1 word, patacake, bye bye, peekaboo Playful Zombie Baby: walking at you, snapping pincers, repeating one word over and over (brrraaaaains), and just wants to play patacake and peekaboo before waving bye bye. 15 months: walks well, imitates, controlled release of blocks (can stack 2) Little Sister Baby: wants to be just like big sister, walks confidently to the blocks and imitates making a 2 block tower 18 months: Throw, scribble, 4 block tower, 1 step command, uses spoon/cup, points to parts of body Sir Charming Baby: needs to get note to Rapunzel so scribbles note on paper to throw into high 4 block tower, catapult has cup on end, shoves note in with spoon, and throws note at tower, hitting Rapunzel in the face 2 years: Run, stairs (1 foot at a time), 20-50 words, 2 step command, parallel play Bad Twins: mom gives two commands to twin boys to run to the stairs, then walk up the 25 stairs. Each walks up the 25 stairs not helping the other. 3 years: Jump, Tricycle, dresses self (shirt, pants, shoes), full name, “you, me, I” James Bond Baby: springs into action … jumps into 3-piece suit, stands in front of mirror and says full name, jumps on tricycle. “You.Me. I,” is his pickup line. 4 years: Stairs (alternating feet), hop, undresses, 1 foot (4 seconds), 4 word phrases (complete sentences), cooperative play Bedtime Story Baby: really wants story time, so runs up stairs, hops on one foot to undress, so she and mom can read a story together. A Wrinkle in Time. 5 years: Skip, Tie shoes, Difference between reality/fantasy Oz Baby: ties ruby shoes, skips down Yellow Brick Road back to Kansas Developmental assessment Primitive reflexes Mnemonic: MPRAG M Moro P Placing reflex R Rooting A Aton
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Development
n one foot to undress, so she and mom can read a story together. A Wrinkle in Time. 5 years: Skip, Tie shoes, Difference between reality/fantasy Oz Baby: ties ruby shoes, skips down Yellow Brick Road back to Kansas <span>Developmental assessment Primitive reflexes Mnemonic: MPRAG M Moro P Placing reflex R Rooting A Atonic neck reflex G Grasp reflex Head circumference with age · Remember 3, 9, and multiples of 5: Newborn 35 cm 3 mos 40 cm 9 mos 45 cm 3 yrs 50 cm 9 yrs 5
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Development
13; Developmental assessment Primitive reflexes Mnemonic: MPRAG M Moro P Placing reflex R Rooting A Atonic neck reflex G Grasp reflex <span>Head circumference with age · Remember 3, 9, and multiples of 5: Newborn 35 cm 3 mos 40 cm 9 mos 45 cm 3 yrs 50 cm 9 yrs 55 cm Head Circumference 336:633 Infants increase their head circumference by 12 centimeters during the first year of life as they start with an average of 35 centimeters and end up with an average of 47 centimeters. To remember the rates of increase at various months of the first year, we can use the above mnemonic; * It means that during the first three months infants will gain six centimeters increase in OFC (occipitofrontal circumference) which means 2 centimeters per month. * The next three months the rate is three centimeters in three months which means 1 cm per month. * The next six months the rate is three centimeters in six months which means 0.5 cm per month. Length and height values and acceleration Although there are a number of formulas that facilitate the estimation o
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Development
hs the rate is three centimeters in three months which means 1 cm per month. * The next six months the rate is three centimeters in six months which means 0.5 cm per month. <span>Length and height values and acceleration Although there are a number of formulas that facilitate the estimation of the expected length or height at a given age but this mnemonic is incredibly easy to remember. Just remember multiples of the number 5 Birth 1 Year 4 Years 8 Years 12 Years 50 cm 75 cm 100 cm 125 cm 150 cm 25cm/yr* 10 cm/yr* 5cm/yr* 5cm/yr* Weights of children with age Newborn 3 kg 6 mos 6 kg (2x birth wt at 6 mos) 1 y
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Development
25cm/yr* 10 cm/yr* 5cm/yr* 5cm/yr* <span>Weights of children with age Newborn 3 kg 6 mos 6 kg (2x birth wt at 6 mos) 1 yr 10 kg (3x birth wt at 1 yr) 3 yrs 15 kg (odd yrs, add 5 kg until 11 yrs) 5 yrs 20 kg 7 yrs 25 kg 9 yrs 30 kg 11 yrs 35 kg (add 10 kg thereafter) 13 yrs 45 kg 15 yrs 55 kg 17 yrs 65 kg 124 124 rule. 1day birth wt (this is the easy one) 2week regain birth wt 4month 2x birth wt 12month 3x birth wt 24month 4x birth wt <span><body><html>
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Documentation
DOCUMENTATION Admission Note (Template) Paediatric History and Physical Examination (as previous), and: INVESTIGATIONS • Blood work: CBC, electrolytes, glucose, renal function, liver function • Microbiology: blood, urine, CSF, nasal, stool cultures • Imaging: x‐ray, ultrasounds, CT, MRI • Pathology: if relevant IMPRESSION/ASSESSMENT (IMP) This is a (year old) (sex) [who is previously healthy] or [with a history of XYZ] presenting with (brief summary of pertinent positive/ negative symptoms on history, signs on physical examination and relevant investigations) with a most likely diagnosis of _____________. DIFFERENTIAL DIAGNOSIS (DDX) May chose to use broad categories by system or process when considering specific diagnoses (i.e., use of VITAMINS ACD acronym) Vascular, Infectious/Inflammatory, Traumatic/Toxin, Autoimmune/ Acquired, Metabolic/Medication, Iatrogenic/Idiopathic, Neoplastic, Social, Allergic, Congenital, Degenerative, Endocrine MANAGEMENT PLAN/ADMISSION ORDERS (PLAN) • Admit: Admit to (your service) under (your consultant today). • Diagnosis: This is what you suspect they have. (e.g., Asthma) • Diet: DAT (diet as tolerated) NPO (nothing per os/by mouth; if going for surgery or procedures), Breast feed ad lib, Formula, Tube feeds (NG‐tube, G‐tube, GJ‐tube) • Activity: AAT (Activity as Tolerated), bedrest • Vital Signs: VS (Vital Signs q8‐12h = HR, RR, BP, O2 sat, Temp), VS q4h (if particularly sick patient requiring more frequent vitals), Special parameters (e.g., Neurological vitals) • Monitoring: ECG, oxygen saturation, Ins & Outs, daily weights • Investigations o Bloodwork (Hematology, Biochemistry) o Microbiology o Imaging o Consults • Drugs o Past: Medication Reconciliation – all regular medications (may not need all; e.g., no need for previous PO antibiotics if starting IV) o Present: what does patient need now o Future: anticipate what patient may need; e.g., fever, nausea, pain, stools Progress Note (Template) (Service) Progress Note Date, Time ID Age, sex with a history of (non‐active/chronic issues) admitted with (list active/acut
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Documentation
egular medications (may not need all; e.g., no need for previous PO antibiotics if starting IV) o Present: what does patient need now o Future: anticipate what patient may need; e.g., fever, nausea, pain, stools <span>Progress Note (Template) (Service) Progress Note Date, Time ID Age, sex with a history of (non‐active/chronic issues) admitted with (list active/acute issues for why the patient is admitted). Could also include a list of recent events that occurred since the most recent note. SUBJECTIVE • How was patient overnight, how they feel that day, any new concerns from the patient/parent • What has changed since the previous note? Does the patient have any new symptoms? Any pain? How is the patient coping with the active symptoms, progression, better/worse. • Ask the parents and patient’s nurse: behaviour, activity, sleep, appetite, in and outs. OBJECTIVE Vitals: HR, BP, RR, SaO2, Temp, daily weight, pain I/O: Inputs (Diet, IVF), Output (U/O, BM/Diarrhea, Vx, Drains), fluid balance General: what the patient is doing, appearance, behaviour, cognition, cooperation, disposition P/E: focused physical exam of system involved plus CVS, RESP, ABDO as it is common for hospitalized patients to develop problems in these regions. INVESTIGATIONS New lab results, imaging or diagnostic tests/ interventions and relevant results still pending MEDS Reviewed daily regarding changes such as new/held/discontinued/ restarted (e.g. Ampicillin day 2/10) IMPRESSION/ASSESSMENT (IMP) Summarize what the new findings mean, what progress is being made. Stable vs. Unstable? Improved vs. Worsened? Waiting investigations/ consult? Differential diagnosis if anything has been ruled in/out? PLAN (P) 1. Issue (1) plan (e.g., UTI on Day 2 of Empiric Abx, likely 14 day course required, await urine C&S) 2. Issue (2) plan 3. Issue (3) plan 4. Disposition – plans for home, transfer Discharge Summary (Template) Check patient’s name, medical record number, date of birth, date of admission, date of discharge, most responsible physician (MRP), ref
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Documentation
t? PLAN (P) 1. Issue (1) plan (e.g., UTI on Day 2 of Empiric Abx, likely 14 day course required, await urine C&S) 2. Issue (2) plan 3. Issue (3) plan 4. Disposition – plans for home, transfer <span>Discharge Summary (Template) Check patient’s name, medical record number, date of birth, date of admission, date of discharge, most responsible physician (MRP), referring physician name. FINAL DISCHARGE DIAGNOSIS • Often only one diagnosis is responsible for admission (i.e. vasoocclusive crisis, asthma exacerbation, bronchiolitis or Kawasaki Disease) • However sometimes there are associated diagnoses (i.e. Gastroenteritis with dehydration and renal failure, osteomyelitis with bacteremia) OTHER DIAGNOSIS (nonactive or those affecting hospital stay) Other diagnoses requiring treatment during hospitalization or underlying medical diagnoses existing prior to admission HISTORY OF PRESENTING ILLNESS (Name) is a (year old) (sex) [who is previously healthy] or [with a past medical history of XYZ] who presented with (X) day history of (summary of pertinent positive and negative symptoms on history and other relevant/contributing elements of birth history, development, past investigations/treatment, immunizations as appropriate). Significant signs on initial physical examination included__________. In the ER, management included _______________. COURSE IN HOSPITAL (Name) was admitted to (name of service and ward)… [and describe briefly the events and progression of illness while in hospital including results and management. If the child has multiple medical issues, this section can be done by system (cardiovascular, respiratory, fluids and nutrition, ID, CNS, etc). List significant/complex investigations (with results) under a separate heading. At discharge, describe current symptoms, physical examination and pending results. DISCHARGE MEDICATIONS Drug name, dose, route, dosing interval frequency, and duration DISCHARGE GENERAL INSTRUCTIONS AND FOLLOWUP All discharge summaries must include at least 3 essential elements 1. Discharge treatment plan including duration 2. Follow‐up with primary care physician in… (specify a reasonable time frame) 3. Seek medical attention if… May include other referrals and follow‐up appointments as necessary, pending investigations and other community resources Handover At Sick Kids, IPASS is the format used for handover. • Illness severity o Stable / Watcher / Unstable • Patient Summary o Summary state
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
Documentation
rimary care physician in… (specify a reasonable time frame) 3. Seek medical attention if… May include other referrals and follow‐up appointments as necessary, pending investigations and other community resources <span>Handover At Sick Kids, IPASS is the format used for handover. • Illness severity o Stable / Watcher / Unstable • Patient Summary o Summary statement o Events leading up to admission o Hospital course o On‐going assessment o Plan • Action Items o To‐do list o Timeline and ownership • Situational awareness and contingency planning o Know what’s going on o Plan for what might happen • Synthesis by receiver o Receiver summarizes what was heard o Asks questions o Restates key actions/to do items<span><body><html>
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
CLIPP 11 - Kawasaki
11. 5-year-old with fever and adenopathy - Jason January 27, 2017 2:09:56 PM EST Knowledge Irritability in a Child Irritability may be the only way that a young child can express pain or discomfort from any source, including: Meningeal irritation Headache from intracranial irritation Simple exhaustion Pediatric Vital Signs As a child gets older, the normal ranges for vital signs change, making it important to look at ageappropriate reference values. The normal hea
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
CLIPP 11 - Kawasaki
Irritability in a Child Irritability may be the only way that a young child can express pain or discomfort from any source, including: Meningeal irritation Headache from intracranial irritation Simple exhaustion <span>Pediatric Vital Signs As a child gets older, the normal ranges for vital signs change, making it important to look at ageappropriate reference values. The normal heart rate for a 5-year-old is 80 to 100 beats per minute. Rashes Associated with Fever (Part 1) Children get many different kinds of rashes-many, though not all, related to infections. Below are descriptions and photos of rashe
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
CLIPP 11 - Kawasaki
; Pediatric Vital Signs As a child gets older, the normal ranges for vital signs change, making it important to look at ageappropriate reference values. The normal heart rate for a 5-year-old is 80 to 100 beats per minute. <span>Rashes Associated with Fever (Part 1) Children get many different kinds of rashes-many, though not all, related to infections. Below are descriptions and photos of rashes associated with fever. Cho Sooyoung - sooyoung.cho@mail.utoronto.ca 1/15 Enterovirus Usually erythematous and maculopapular, and may involve the palms and soles. Infrequently, it can be petechial. In hand-foot-and-mouth disease (caused by Coxsackie virus), presents as a vesicular rash on the hands and feet and with ulcers in the mouth. Usually seen in late summer and early fall. While the fever associated with enteroviruses may be high, it usually lasts only a few days. Erythema infectiosum Also called fifth disease, this is caused by parvovirus B19. There is frequently an associated low-grade fever (37.8-38.3 degrees C, or 100
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
CLIPP 11 - Kawasaki
presents as a vesicular rash on the hands and feet and with ulcers in the mouth. Usually seen in late summer and early fall. While the fever associated with enteroviruses may be high, it usually lasts only a few days. <span>Erythema infectiosum Also called fifth disease, this is caused by parvovirus B19. There is frequently an associated low-grade fever (37.8-38.3 degrees C, or 100-101 degrees F), with a rash appearing seven to ten days later. The characteristic rash starts as facial erythema-the "slapped cheek" appearance. This can spread to the trunk and have an erythematous macular appearance. Central clearing of the rash appears, giving a lacy appearance. The rash often lasts longest on the extremities, where it has a lacy, reticular appearance. People with fifth disease can also develop pain and swelling in their joints (polyarthropathy syndrome). Individuals with underlying immune deficiencies who are exposed to this virus are at risk for developing aplastic anemia. Measles After a prodrome of fever (over 38.3 C, or 101 F), cough, coryza, and conjunctivitis, this maculopapular rash starts on the neck, behind the ears, and along
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
CLIPP 11 - Kawasaki
le with fifth disease can also develop pain and swelling in their joints (polyarthropathy syndrome). Individuals with underlying immune deficiencies who are exposed to this virus are at risk for developing aplastic anemia. <span>Measles After a prodrome of fever (over 38.3 C, or 101 F), cough, coryza, and conjunctivitis, this maculopapular rash starts on the neck, behind the ears, and along the hairline. The rash spreads downward, reaching the feet in two or three days. The initial rash appears on the buccal mucosa as red lesions with bluish white spots in the center (known as Koplik spots). These have frequently disappeared by the time the patient presents to medical attention. Immunization is very effective in preventing this infection. All photos in this case showing disease manifestations are courtesy of Gary Williams, MD, and the University of Wisconsin teaching file. Hyperlink "hands "
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
CLIPP 11 - Kawasaki
erial is not included in this Summary, please open Case to review. Hyperlink " Measles " This Multimedia material is not included in this Summary, please open Case to review. Rashes Associated with Fever (Part 2) <span>Meningococcemia Caused by the bacteria Neisseria meningitidis, onset is abrupt and accompanied by fever, chills, malaise, and prostration. The initial rash may be urticarial, maculopapular, or petechial (marked by small, purplish, hemorrhagic spots). In fulminant cases, it can become purpuric, marked by large hemorrhages into the skin. Immunization is effective in preventing this infection. Roseola This macular or maculopapular rash, also called exanthem subitum, starts on the trunk and spreads to the arms and neck. There is usually less involvement of
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
CLIPP 11 - Kawasaki
aculopapular, or petechial (marked by small, purplish, hemorrhagic spots). In fulminant cases, it can become purpuric, marked by large hemorrhages into the skin. Immunization is effective in preventing this infection. <span>Roseola This macular or maculopapular rash, also called exanthem subitum, starts on the trunk and spreads to the arms and neck. There is usually less involvement of the face and legs. The rash is preceded by three or four days of high fevers, which end as the rash appears. Usually seen in children less than two years old. 3/15 Scarlet fever This rash, caused by infection with group A Streptococcus, consists of very fine papules, often described as feeling like sandpaper. It is er
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
CLIPP 11 - Kawasaki
s and neck. There is usually less involvement of the face and legs. The rash is preceded by three or four days of high fevers, which end as the rash appears. Usually seen in children less than two years old. 3/15 <span>Scarlet fever This rash, caused by infection with group A Streptococcus, consists of very fine papules, often described as feeling like sandpaper. It is erythematous, but blanches. The rash starts in the groin, axillae, and neck, but rapidly spreads. The fever can be high, and the disease is usually self-limited, lasting less than 10 days. It is important to treat with antibiotics to prevent non-suppurative complications of strep, including rheumatic fever. Varicella The rash, also known as chicken pox, starts on the trunk and spreads to the extremities and head. Each lesion progresses from an erythematous macule to pap
| status | not read | reprioritisations | ||
|---|---|---|---|---|
| last reprioritisation on | suggested re-reading day | |||
| started reading on | finished reading on |
CLIPP 11 - Kawasaki
reads. The fever can be high, and the disease is usually self-limited, lasting less than 10 days. It is important to treat with antibiotics to prevent non-suppurative complications of strep, including rheumatic fever. <span>Varicella The rash, also known as chicken pox, starts on the trunk and spreads to the extremities and head. Each lesion progresses from an erythematous macule to papule to vesicle to pustule, and then crusts over. Lesions at various stages of development are seen in the same area of the body. There is usually a mild fever. The disease is self-limited, lasting about a week. Immunization is effective in preventing this infection. Hyperlink " Meningococcemia " This Multimedia material is not included in this Summary, please open Case to review. Hyperlink " Roseola " This Mu
Flashcard 1473443663116
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itxactly, without any approximation or limits on their size. On the other hand, float objects can represent a wide range of fractional numbers, but not all numbers can be represented exactly, and there are minimum and maximum values. Therefore, <span>float values should be treated as approximations to real values.<span><body><html>
Original toplevel document
2.1 Introductionming languages: a "floating point" representation. While the details of how numbers are represented is not a topic for this text, some high-level differences between int and float objects are important to know. In particular, <span>int objects represent integers exactly, without any approximation or limits on their size. On the other hand, float objects can represent a wide range of fractional numbers, but not all numbers can be represented exactly, and there are minimum and maximum values. Therefore, float values should be treated as approximations to real values. These approximations have only a finite amount of precision. Combining float values can lead to approximation errors; both of the following expressions would evaluate to 7 if not fo
Flashcard 1473446022412
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itIn general, the underlying idea of data abstraction is to identify a basic set of operations in terms of which all manipulations of values of some kind will be expressed, and then to use only those operations in manipulating the data. By restricting the use of operations in this way, it is much easier to change the representation of abstract data without changing the behavior of a program.
Original toplevel document
2.2 Data Abstractionefore continuing with more examples of compound data and data abstraction, let us consider some of the issues raised by the rational number example. We defined operations in terms of a constructor rational and selectors numer and denom . <span>In general, the underlying idea of data abstraction is to identify a basic set of operations in terms of which all manipulations of values of some kind will be expressed, and then to use only those operations in manipulating the data. By restricting the use of operations in this way, it is much easier to change the representation of abstract data without changing the behavior of a program. For rational numbers, different parts of the program manipulate rational numbers using different operations, as described in this table. Parts of the program that... Treat rationals
Flashcard 1473448381708
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itn>In general, the underlying idea of data abstraction is to identify a basic set of operations in terms of which all manipulations of values of some kind will be expressed, and then to use only those operations in manipulating the data. By restricting the use of operations in this way, it is much easier to change the representation of abstract data without changing the behavior of a program.<span><body><html>
Original toplevel document
2.2 Data Abstractionefore continuing with more examples of compound data and data abstraction, let us consider some of the issues raised by the rational number example. We defined operations in terms of a constructor rational and selectors numer and denom . <span>In general, the underlying idea of data abstraction is to identify a basic set of operations in terms of which all manipulations of values of some kind will be expressed, and then to use only those operations in manipulating the data. By restricting the use of operations in this way, it is much easier to change the representation of abstract data without changing the behavior of a program. For rational numbers, different parts of the program manipulate rational numbers using different operations, as described in this table. Parts of the program that... Treat rationals
Flashcard 1473450741004
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itWe follow the same recursive analysis of the problem as we did while counting: partitioning n using integers up to m involves either partitioning n-m using integers up to m , or partitioning n using integers up to m-1 . For base cases, we find that 0 has an empty partition, while partitioning a negative integer or using parts smaller than 1 is impossible.</sp
Flashcard 1473455459596
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itPython does not have a separate character type; any text is a string, and strings that represent single characters have a length of 1.
Flashcard 1473457818892
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itThe tree is a fundamental data abstraction that imposes regularity on how hierarchical values are structured and manipulated.
Flashcard 1473460178188
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Flashcard 1473462537484
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itAny tree contained within a tree is called a sub-tree of that tree (such as a branch of a branch)
Flashcard 1473464896780
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itStep 2 Problem statement. Develop a detailed statement of the mathematical problem to be solved with a computer program.
Original toplevel document (pdf)
cannot see any pdfsFlashcard 1473467256076
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itStep 4 Algorithm. Design the step-by-step procedure in a top-down process that decomposes the overall problem into subordinate problems. The subtasks to solve the latter are refined by designing an itemized list of steps to be programmed. This list o f tasks is the structure plan and is written in pseudo- code (i.e., a combination of English, mathematics, and anticipated MATLAB commands). The goal is a plan that is understandable and easily translated into a computer language.
Original toplevel document (pdf)
cannot see any pdfsFlashcard 1473469615372
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itA binary tree is either a leaf or a sequence of at most two binary trees.
Flashcard 1473471974668
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itA list is depicted as adjacent boxes that contain the elements of the list. Primitive values such as numbers, strings, boolean values, and None appear within an element box. Composite values, such as function values and other lists, are indicated by an arrow.<
Flashcard 1473479052556
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itA linked list is a pair containing the first element of the sequence (in this case 1) and the rest of the sequence (in this case a representation of 2, 3, 4). The second element is also a linked list. The rest of the inner-most linked list containing only 4 is 'empty' , a value that represents an em
Flashcard 1473481411852
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open it1. A probability value must be nonnegative (i.e., zero or positive).
Original toplevel document (pdf)
cannot see any pdfsFlashcard 1473483771148
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open it3. For any two mutually exclusive events, the probability that one or the other occurs is the sum of their individual probabilities.
Original toplevel document (pdf)
cannot see any pdfsFlashcard 1473488489740
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itThe basic idea of data abstraction is to structure programs so that they operate on abstract data. That is, our programs should use data in such a way as to make as few assumptions about the data as possible
Original toplevel document
2.2 Data Abstractionwe can make an abstraction that separates the way the function is used from the details of how the function is implemented. Analogously, data abstraction isolates how a compound data value is used from the details of how it is constructed. <span>The basic idea of data abstraction is to structure programs so that they operate on abstract data. That is, our programs should use data in such a way as to make as few assumptions about the data as possible. At the same time, a concrete data representation is defined as an independent part of the program. These two parts of a program, the part that operates on abstract data and the part that defines a concrete representation, are connected by a small set of functions that implement abs
Flashcard 1473490849036
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itThe built-in functions sum , min , and max are all examples of aggregation functions.
Flashcard 1473493994764
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itThe root value of a sub-tree of a tree is called a node (or node value) in that tree.
Flashcard 1473496354060
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itStep 6 Evaluation. Test all of the options and conduct a validation study of the program. For example, compare results with other programs that do similar tasks, compare with experimental data if appropriate, and compare
Original toplevel document (pdf)
cannot see any pdfsFlashcard 1473498713356
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open it2. The sum of the probabilities across all events in the entire sample space must be 1.0 (i.e., one of the events in the space must happen, otherwise the space does not exhaust all possibilities).
Original toplevel document (pdf)
cannot see any pdfsFlashcard 1473503431948
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itThe values we have used so far are instances of a small number of native data types that are built into the Python language. Native data types have the following properties: There are expressions that evaluate to values of native types, called literals. There are built-in functions and operators to manipulate values of native types. The int class is the native data type used to represent integers. Integer literals (sequences of adjac
Original toplevel document
2.1 Introductioninstances of the int class. These two values can be treated similarly. For example, they can both be negated or added to another integer. The built-in type function allows us to inspect the class of any value. >>> type(2) <span>The values we have used so far are instances of a small number of native data types that are built into the Python language. Native data types have the following properties: There are expressions that evaluate to values of native types, called literals. There are built-in functions and operators to manipulate values of native types. The int class is the native data type used to represent integers. Integer literals (sequences of adjacent numerals) evaluate to int values, and mathematical operators manipulate these values. >>> 12 + 3000000000000000000000000 3000000000000000000000012 Python includes three native numeric types: integers ( int ), real numbers ( float ), and complex numbers ( c
Flashcard 1473505791244
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open ithave used so far are instances of a small number of native data types that are built into the Python language. Native data types have the following properties: There are expressions that evaluate to values of native types, called literals. <span>There are built-in functions and operators to manipulate values of native types. The int class is the native data type used to represent integers. Integer literals (sequences of adjacent numerals) evaluate to int values, and mathematical operators manipulate these
Original toplevel document
2.1 Introductioninstances of the int class. These two values can be treated similarly. For example, they can both be negated or added to another integer. The built-in type function allows us to inspect the class of any value. >>> type(2) <span>The values we have used so far are instances of a small number of native data types that are built into the Python language. Native data types have the following properties: There are expressions that evaluate to values of native types, called literals. There are built-in functions and operators to manipulate values of native types. The int class is the native data type used to represent integers. Integer literals (sequences of adjacent numerals) evaluate to int values, and mathematical operators manipulate these values. >>> 12 + 3000000000000000000000000 3000000000000000000000012 Python includes three native numeric types: integers ( int ), real numbers ( float ), and complex numbers ( c
Flashcard 1473507364108
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itIn general, we can express abstract data using a collection of selectors and constructors, together with some behavior conditions. As long as the behavior conditions are met (such as the division property above), the selectors and constructors constitute a valid representation of a kind of data. The implementation
Original toplevel document
2.2 Data Abstractionenom . In addition, the appropriate relationship must hold among the constructor and selectors. That is, if we construct a rational number x from integers n and d , then it should be the case that numer(x)/denom(x) is equal to n/d . <span>In general, we can express abstract data using a collection of selectors and constructors, together with some behavior conditions. As long as the behavior conditions are met (such as the division property above), the selectors and constructors constitute a valid representation of a kind of data. The implementation details below an abstraction barrier may change, but if the behavior does not, then the data abstraction remains valid, and any program written using this data abstraction will remain correct. This point of view can be applied broadly, including to the pair values that we used to implement rational numbers. We never actually said much about what a pair was, only that the la
Flashcard 1473512082700
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itSequences contain smaller sequences within them. A slice of a sequence is any contiguous span of the original sequence, designated by a pair of integers. As with the range constructor, the first integer indicates the starting index of the sli
Flashcard 1473516801292
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itthe add function in the operator module (and the + operator) yields a list that is the concatenation of the added arguments
Original toplevel document
2.3 Sequenceshe built-in len function returns the length of a sequence. Below, digits is a list with four elements. The element at index 3 is 8. >>> digits = [1, 8, 2, 8] >>> len(digits) 4 >>> digits[3] 8 Additionally, <span>lists can be added together and multiplied by integers. For sequences, addition and multiplication do not add or multiply elements, but instead combine and replicate the sequences themselves. That is, the add function in the operator module (and the + operator) yields a list that is the concatenation of the added arguments. The mul function in operator (and the * operator) can take a list and an integer k to return the list that consists of k repetitions of the original list. >>> [2, 7] + digits * 2 [2, 7, 1, 8, 2, 8, 1, 8, 2, 8] Any values can be included in a list, including another list. Element selection can be applied multiple times in or
Flashcard 1473519160588
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itThe mul function in operator (and the * operator) can take a list and an integer k to return the list that consists of k repetitions of the original list.
Original toplevel document
2.3 Sequenceshe built-in len function returns the length of a sequence. Below, digits is a list with four elements. The element at index 3 is 8. >>> digits = [1, 8, 2, 8] >>> len(digits) 4 >>> digits[3] 8 Additionally, <span>lists can be added together and multiplied by integers. For sequences, addition and multiplication do not add or multiply elements, but instead combine and replicate the sequences themselves. That is, the add function in the operator module (and the + operator) yields a list that is the concatenation of the added arguments. The mul function in operator (and the * operator) can take a list and an integer k to return the list that consists of k repetitions of the original list. >>> [2, 7] + digits * 2 [2, 7, 1, 8, 2, 8, 1, 8, 2, 8] Any values can be included in a list, including another list. Element selection can be applied multiple times in or
Flashcard 1473523879180
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Flashcard 1473526238476
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itStep 1 Problem analysis. The context of the proposed investigation must be es- tablished to provide the proper motivation for the d esign of a computer program. The designer must fully recognize the need and must develop an understanding of the nature of the problem to be solved.
Original toplevel document (pdf)
cannot see any pdfsFlashcard 1473528597772
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itStep 3 Processing scheme. Define the inputs required and the outputs to be pro- duced by the p rogram.
Original toplevel document (pdf)
cannot see any pdfsFlashcard 1473530957068
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itStep 5 Program algorithm. Translate or convert the algorithm into a computer language (e.g., MATLAB) and debug the syntax errors until the tool executes successfully.
Original toplevel document (pdf)
cannot see any pdfsFlashcard 1473533316364
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itStep 7 Application. Solve the problems the program was designed to solve. If the program is well designed and useful, it can be saved in your working directory (i.e., in your user-developed toolbox) for future use
Original toplevel document (pdf)
cannot see any pdfsFlashcard 1473535675660
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itLinked lists have recursive structure: the rest of a linked list is a linked list or 'empty'
Flashcard 1473538034956
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itThe general technique of isolating the parts of a program that deal with how data are represented from the parts that deal with how data are manipulated is a powerful design methodology called data abstraction.
Original toplevel document
2.2 Data Abstractionta enables us to increase the modularity of our programs. If we can manipulate geographic positions as whole values, then we can shield parts of our program that compute using positions from the details of how those positions are represented. <span>The general technique of isolating the parts of a program that deal with how data are represented from the parts that deal with how data are manipulated is a powerful design methodology called data abstraction. Data abstraction makes programs much easier to design, maintain, and modify. Data abstraction is similar in character to functional abstraction. When we create a functional abstraction, the details of how a function is implemented can be suppressed, and the p
Flashcard 1473540394252
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Flashcard 1473542753548
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itPartition trees. Trees can also be used to represent the partitions of an integer. A partition tree for n using parts up to size m is a binary (two branch) tree that represents the choices taken during computation. In a non-leaf partition tree: the left (index 0) branch contains all ways of partitioning n using at least one m , the right (index 1) branch contains partitions using parts up to m-
Flashcard 1473545112844
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itto represent the partitions of an integer. A partition tree for n using parts up to size m is a binary (two branch) tree that represents the choices taken during computation. In a non-leaf partition tree: the left (index 0) branch contains <span>all ways of partitioning n using at least one m , the right (index 1) branch contains partitions using parts up to m-1 , and the root value is m .<span><body><html>
Flashcard 1473547472140
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open itize m is a binary (two branch) tree that represents the choices taken during computation. In a non-leaf partition tree: the left (index 0) branch contains all ways of partitioning n using at least one m , the right (index 1) branch contains <span>partitions using parts up to m-1 , and the root value is m .<span><body><html>
Flashcard 1473549831436
| status | not learned | measured difficulty | 37% [default] | last interval [days] | |||
|---|---|---|---|---|---|---|---|
| repetition number in this series | 0 | memorised on | scheduled repetition | ||||
| scheduled repetition interval | last repetition or drill |
Parent (intermediate) annotation
Open ithoices taken during computation. In a non-leaf partition tree: the left (index 0) branch contains all ways of partitioning n using at least one m , the right (index 1) branch contains partitions using parts up to m-1 , and the root value is <span>m .<span><body><html>
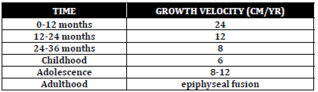
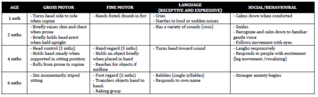
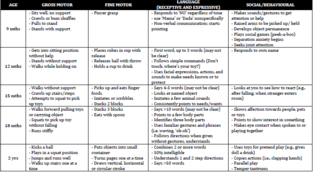
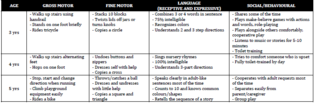
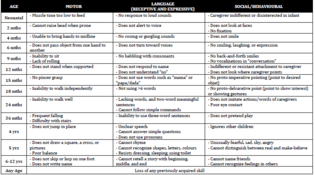 ...
...